Tachycardia is a condition characterized by an abnormally fast heart rate, typically over 100 beats per minute. While it can occur in various forms, understanding whether tachycardia is atrial or ventricular is critical for determining its cause, symptoms, and treatment options.
This article will explore the differences between atrial and ventricular tachycardia, their mechanisms, causes, symptoms, diagnosis, and treatment.
What Is Tachycardia?
Tachycardia occurs when the heart beats too quickly. The heart has a natural pacemaker, the sinoatrial (SA) node, which controls the rhythm by sending electrical impulses that stimulate the heart muscle to contract. These impulses normally result in a heart rate between 60 and 100 beats per minute. However, when the electrical impulses are disrupted, the heart may beat faster than normal, leading to tachycardia.
Tachycardia can originate from different parts of the heart: the atria (upper chambers of the heart) or the ventricles (lower chambers of the heart). Understanding whether tachycardia is atrial or ventricular is essential for proper management and treatment.
Atrial Tachycardia: An Overview
Atrial tachycardia occurs when the electrical signals that regulate the heartbeat begin in the atria. It is often associated with an abnormality in the electrical system of the heart that causes the atria to beat rapidly and irregularly.
Causes of Atrial Tachycardia
Atrial tachycardia can be caused by several factors, including:
Heart Disease: Conditions such as hypertension, coronary artery disease, and heart failure can increase the risk of atrial tachycardia.
Electrolyte Imbalances: Imbalances in potassium, magnesium, or calcium levels can affect the heart’s electrical impulses, leading to tachycardia.
Structural Changes in the Heart: Conditions like atrial fibrillation or atrial flutter can predispose a person to atrial tachycardia.
Excessive Stimulation: Overuse of stimulants such as caffeine, alcohol, or recreational drugs can trigger atrial tachycardia.
Genetic Factors: Some people may have a genetic predisposition to develop atrial arrhythmias, including tachycardia.
Symptoms of Atrial Tachycardia
The symptoms of atrial tachycardia can vary from person to person, but common symptoms include:
- Palpitations (a feeling of a fast or irregular heartbeat)
- Shortness of breath
- Dizziness or lightheadedness
- Chest discomfort or tightness
- Fatigue
In some cases, atrial tachycardia may not cause any symptoms and may only be detected during a routine medical examination or an ECG (electrocardiogram).
Diagnosis of Atrial Tachycardia
To diagnose atrial tachycardia, a healthcare provider will typically conduct an ECG, which records the electrical activity of the heart. The ECG will show rapid, abnormal electrical impulses originating from the atria. Additional tests, such as an echocardiogram, may be performed to assess the heart’s structure and function.
Treatment of Atrial Tachycardia
The treatment of atrial tachycardia depends on its severity, the underlying cause, and the overall health of the patient.
Some common treatment options include:
Medications: Antiarrhythmic drugs such as beta-blockers or calcium channel blockers may be prescribed to regulate the heart rate.
Electrical Cardioversion: In more severe cases, a procedure called electrical cardioversion may be used to restore normal rhythm.
Catheter Ablation: If atrial tachycardia is recurrent and difficult to manage with medications, catheter ablation may be performed. This procedure involves using radiofrequency energy to destroy the abnormal tissue causing the arrhythmia.
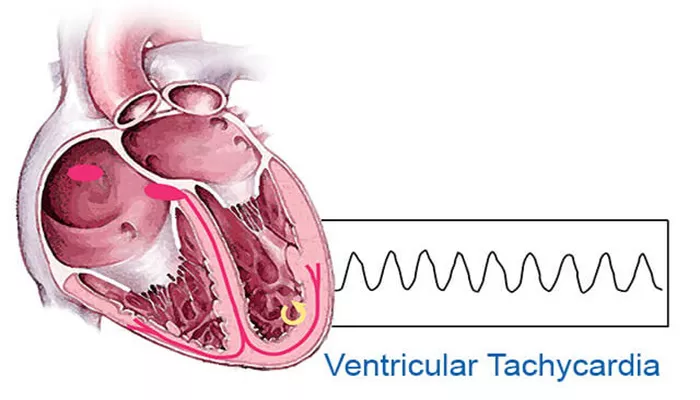
Ventricular Tachycardia: An Overview
Ventricular tachycardia is a more serious form of tachycardia that originates in the ventricles, the lower chambers of the heart. This condition is often associated with heart disease and can be life-threatening, especially if it leads to ventricular fibrillation.
Causes of Ventricular Tachycardia
Ventricular tachycardia is most commonly caused by:
Coronary Artery Disease: A blockage in the coronary arteries can lead to a reduced blood supply to the heart muscle, increasing the risk of ventricular tachycardia.
Previous Heart Attack: A heart attack can damage the heart muscle, creating scar tissue that disrupts the electrical signals and can trigger ventricular tachycardia.
Heart Failure: People with heart failure are at a higher risk of developing ventricular tachycardia.
Electrolyte Imbalances: Like atrial tachycardia, electrolyte imbalances can affect the electrical impulses in the heart, leading to ventricular tachycardia.
Inherited Arrhythmias: Some inherited conditions, such as Long QT syndrome or Brugada syndrome, can cause abnormal electrical activity in the ventricles, leading to tachycardia.
Symptoms of Ventricular Tachycardia
Ventricular tachycardia can cause severe symptoms, including:
- Dizziness or fainting (syncope)
- Shortness of breath
- Chest pain or discomfort
- Rapid or irregular heartbeat
- Sudden loss of consciousness
In some cases, if ventricular tachycardia progresses to ventricular fibrillation, it can lead to sudden cardiac arrest, which is a medical emergency requiring immediate attention.
Diagnosis of Ventricular Tachycardia
Ventricular tachycardia is typically diagnosed using an ECG, which will show a rapid and irregular rhythm originating from the ventricles. A healthcare provider may also conduct additional tests such as an echocardiogram or a stress test to evaluate the heart’s function and structure.
Treatment of Ventricular Tachycardia
The treatment of ventricular tachycardia depends on the severity and underlying cause of the condition. Some treatment options include:
Medications: Antiarrhythmic drugs may be prescribed to help control the heart rate and rhythm.
Implantable Cardioverter-Defibrillator (ICD): For people with a high risk of sudden cardiac arrest due to ventricular tachycardia, an ICD may be implanted. This device monitors the heart’s rhythm and can deliver a shock to restore normal rhythm if needed.
Catheter Ablation: In some cases, catheter ablation may be used to destroy the tissue responsible for the abnormal electrical signals in the ventricles.
Emergency Care: If ventricular tachycardia leads to cardiac arrest, immediate treatment with CPR (cardiopulmonary resuscitation) and defibrillation is necessary.
Atrial vs. Ventricular Tachycardia: Key Differences
While both atrial and ventricular tachycardia result in an abnormally fast heart rate, there are several key differences between the two:
Origin: Atrial tachycardia originates in the atria, while ventricular tachycardia originates in the ventricles.
Severity: Ventricular tachycardia is generally considered more dangerous than atrial tachycardia because it can lead to life-threatening complications like sudden cardiac arrest.
Symptoms: Both types of tachycardia can cause palpitations, dizziness, and shortness of breath, but ventricular tachycardia may cause more severe symptoms like chest pain, syncope, or even sudden loss of consciousness.
Treatment: Treatment options for both types of tachycardia include medications, catheter ablation, and electrical cardioversion, but the management of ventricular tachycardia often requires more aggressive interventions, including ICD implantation.
Conclusion
In conclusion, tachycardia can be classified into atrial or ventricular types, depending on where the abnormal electrical impulses originate in the heart. Atrial tachycardia typically arises from the atria and can be managed with medications and ablation, while ventricular tachycardia originates in the ventricles and may require more urgent treatment, such as ICD implantation or catheter ablation. It is crucial for healthcare providers to accurately diagnose the type of tachycardia to determine the best course of treatment and reduce the risk of complications.
Related topics: