Atrial tachycardia is a type of heart arrhythmia, meaning the heart beats too fast due to an abnormal electrical activity in the atria. When discussing heart arrhythmias, it is important to understand the differences between the various types. Focal atrial tachycardia (FAT) and supraventricular tachycardia (SVT) are both conditions that involve rapid heart rates but differ in their origins and mechanisms. In this article, we will explore whether focal atrial tachycardia is the same as SVT, how they differ, and how they are diagnosed and treated.
What Is Focal Atrial Tachycardia (FAT)?
Focal atrial tachycardia (FAT) is a type of arrhythmia that originates from a specific area, or focus, in the atria of the heart.
This focus, usually located in the right atrium or left atrium, generates abnormal electrical impulses that cause the heart to beat faster than normal. FAT typically causes a heart rate that is between 100 to 250 beats per minute.
Unlike other types of arrhythmias, where the abnormal electrical impulses can be widespread across the atria, focal atrial tachycardia originates from a single point of abnormal activity. This focus of electrical signals can be either constant or intermittent, meaning it may occur consistently or in episodes.
What Is Supraventricular Tachycardia (SVT)?
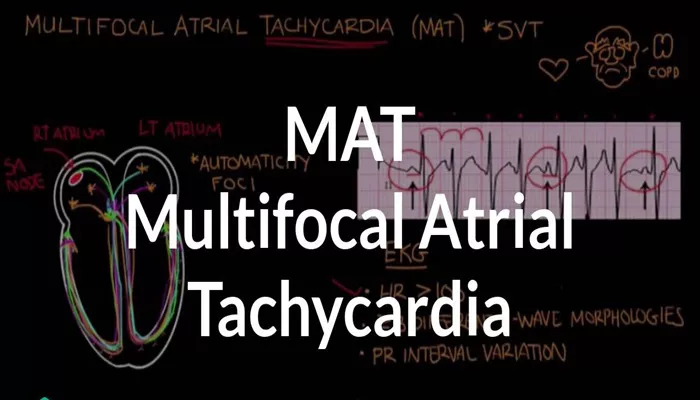
Supraventricular tachycardia (SVT) is a general term used to describe any arrhythmia that originates above the ventricles of the heart, usually from the atria or the atrioventricular (AV) node. The term “supraventricular” means that the arrhythmia occurs above the ventricles. SVT can include several types of arrhythmias, such as atrial fibrillation, atrial flutter, and, of course, focal atrial tachycardia.
SVT is characterized by an abnormally fast heart rate, often exceeding 100 beats per minute, but the specific mechanism and origin can vary.
The heart rate can sometimes reach as high as 300 beats per minute in some cases, particularly in more severe episodes.
Are Focal Atrial Tachycardia and SVT the Same?
While focal atrial tachycardia is technically a form of SVT, the two conditions are not exactly the same. FAT is one type of arrhythmia that falls under the broader category of SVT. The key difference lies in their mechanisms of origin and the way the arrhythmias are triggered.
Origin of the Arrhythmia: FAT arises from a specific, localized area (focus) in the atria. In contrast, SVT can originate from various locations, including the atria, AV node, or other pathways above the ventricles. While FAT is a subset of SVT, not all SVTs are FAT.
Triggering Mechanism: FAT tends to be caused by a single ectopic focus in the atria that fires abnormal electrical impulses.
In contrast, other types of SVT, like AV nodal reentrant tachycardia (AVNRT) or AV reciprocating tachycardia (AVRT), are caused by abnormal electrical circuits in the heart, leading to fast heart rates.
Symptoms of Focal Atrial Tachycardia and SVT
The symptoms of both FAT and other forms of SVT can be quite similar, although the intensity and frequency of symptoms can vary depending on the individual and the severity of the arrhythmia.
Common symptoms of both conditions include:
- Rapid heart rate or palpitations
- Dizziness or lightheadedness
- Shortness of breath
- Fatigue
- Chest discomfort or tightness
- Fainting or near-fainting episodes
In FAT, the symptoms may be more intermittent, with episodes that come and go, while in other forms of SVT, the symptoms may be more constant or occur with sudden onset.
Diagnosis of Focal Atrial Tachycardia and SVT
Diagnosing both FAT and SVT typically involves a combination of patient history, physical examination, and specialized tests. One of the most important diagnostic tools is an electrocardiogram (ECG), which records the electrical activity of the heart.
Electrocardiogram (ECG): During an episode of tachycardia, an ECG can help identify the heart’s rhythm and pinpoint the origin of the abnormal electrical signals. In FAT, the ECG may show a narrow QRS complex and a P-wave that is different in shape compared to normal sinus rhythm.
Holter Monitor: If the arrhythmia is intermittent, a Holter monitor may be used to record the heart’s electrical activity over a 24- or 48-hour period to capture the arrhythmia during an episode.
Electrophysiology Study (EPS): In some cases, a more invasive procedure called an electrophysiology study may be performed to map the electrical pathways in the heart and pinpoint the exact location of the abnormal focus causing the arrhythmia.
Treatment Options for Focal Atrial Tachycardia and SVT
The treatment for FAT and other forms of SVT varies based on the severity of the arrhythmia, the patient’s symptoms, and the underlying causes of the condition. Treatment options include lifestyle changes, medications, and, in some cases, procedures such as catheter ablation.
Medications: Beta-blockers, calcium channel blockers, and anti-arrhythmic drugs may be prescribed to control heart rate, reduce symptoms, and prevent future episodes. For individuals with frequent or severe episodes, these medications can be effective in managing the condition.
Catheter Ablation: In cases where medications are not effective, catheter ablation may be recommended. This procedure involves using a catheter to deliver radiofrequency energy to the specific area in the heart where the abnormal electrical signals are originating. The goal is to destroy the focus of abnormal electrical activity, effectively curing the arrhythmia in many cases.
Cardioversion: If the heart rate is dangerously high or if the patient is experiencing significant symptoms, electrical cardioversion may be used to restore normal rhythm.
Lifestyle Changes: For some individuals, lifestyle modifications, such as avoiding caffeine, alcohol, and stress, can help reduce the frequency of arrhythmia episodes.
Conclusion
While focal atrial tachycardia (FAT) is a form of supraventricular tachycardia (SVT), they are not exactly the same. FAT is a specific type of arrhythmia that originates from a single focus in the atria, whereas SVT is a broader term that encompasses various arrhythmias originating above the ventricles. Both conditions share similar symptoms, but their causes and mechanisms differ. Diagnosing and treating these arrhythmias involves a combination of diagnostic tests and personalized treatment plans, including medications, catheter ablation, and lifestyle changes.
Related topics: