Hyperparathyroidism is a condition in which the parathyroid glands, located near the thyroid in the neck, produce too much parathyroid hormone (PTH). This hormone plays a key role in regulating calcium levels in the body. When these glands become overactive, they release excessive amounts of PTH, which leads to an imbalance of calcium in the blood. This imbalance has several effects on the body, one of the most significant being the development of hypertension, or high blood pressure. In this article, we will explore how hyperparathyroidism contributes to the development of hypertension, the mechanisms behind it, and how it can be managed.
What Is Hyperparathyroidism?
The parathyroid glands are four small glands located behind the thyroid. Their primary function is to produce parathyroid hormone, which helps control calcium levels in the blood. PTH regulates calcium by promoting its release from the bones, increasing calcium absorption in the intestines, and reducing calcium loss through the kidneys.
In hyperparathyroidism, the parathyroid glands secrete too much PTH.
This excess PTH leads to an increase in blood calcium levels, a condition known as hypercalcemia. Hyperparathyroidism can be classified into two types:
Primary Hyperparathyroidism: This occurs when there is an issue within the parathyroid glands themselves, such as a tumor or enlargement.
Secondary Hyperparathyroidism: This occurs as a result of another condition that causes low calcium levels, such as kidney disease, which leads to the overproduction of PTH as a compensatory mechanism.
Regardless of the cause, hyperparathyroidism can have serious consequences, including the development of hypertension.
How Does Hyperparathyroidism Cause Hypertension?
The connection between hyperparathyroidism and hypertension is complex and involves multiple mechanisms. Elevated calcium levels, resulting from excessive PTH production, can have direct and indirect effects on the cardiovascular system, leading to an increase in blood pressure. The following mechanisms explain how hyperparathyroidism contributes to hypertension:
Increased Vascular Resistance One of the main ways hyperparathyroidism leads to hypertension is by increasing vascular resistance. High levels of calcium in the blood can cause blood vessels to constrict, making it harder for blood to flow through them. This constriction increases the resistance the heart must overcome to pump blood throughout the body, resulting in higher blood pressure.
In addition, calcium can influence the function of smooth muscle cells in blood vessels. These muscle cells are responsible for regulating the diameter of blood vessels. When calcium levels are high, these smooth muscles contract more strongly, leading to narrower blood vessels and elevated blood pressure.
Enhanced Sympathetic Nervous System Activity The sympathetic nervous system, which is responsible for the body’s “fight or flight” response, also plays a role in regulating blood pressure. Studies have shown that high calcium levels in the blood can stimulate the sympathetic nervous system, leading to an increase in heart rate and the force of heart contractions. This heightened sympathetic activity can contribute to an increase in blood pressure.
Impaired Kidney Function In people with hyperparathyroidism, excess PTH can affect kidney function. The kidneys play a crucial role in regulating blood pressure by controlling the balance of fluids and electrolytes in the body. When calcium levels are too high, the kidneys may not function properly, leading to fluid retention, which can increase blood volume and subsequently raise blood pressure. Additionally, impaired kidney function can reduce the kidneys’ ability to excrete excess sodium, further contributing to high blood pressure.
Increased Renin-Angiotensin-Aldosterone System (RAAS) Activity The renin-angiotensin-aldosterone system (RAAS) is a hormone system that regulates blood pressure by controlling fluid balance and blood vessel constriction. High calcium levels in the blood can activate this system, leading to an increase in sodium and water retention by the kidneys. This retention increases blood volume, contributing to higher blood pressure. The activation of RAAS can also cause blood vessels to constrict, further elevating blood pressure.
Endothelial Dysfunction The endothelium is the thin layer of cells lining blood vessels, and it plays an important role in regulating blood vessel function. High calcium levels can impair the endothelial cells’ ability to produce nitric oxide, a molecule that helps relax blood vessels and lower blood pressure. When nitric oxide production is reduced, blood vessels are less able to dilate, resulting in increased vascular resistance and higher blood pressure.
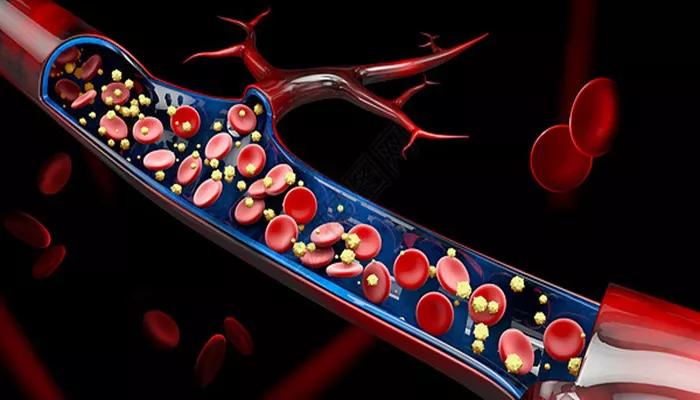
Calcification of Blood Vessels In some cases, prolonged hyperparathyroidism can lead to the calcification (hardening) of blood vessels, particularly in the arteries. The buildup of calcium deposits in the arteries makes them less flexible, which can increase vascular resistance and contribute to higher blood pressure. This process is similar to the development of atherosclerosis, where fatty deposits build up in the blood vessels, leading to stiffness and reduced blood flow.
Symptoms of Hypertension in Hyperparathyroidism
High blood pressure due to hyperparathyroidism often develops gradually, and many people may not experience noticeable symptoms until the hypertension becomes severe. Some common signs and symptoms of hypertension include:
Headaches: Frequent or persistent headaches, particularly in the morning.
Dizziness: Feeling lightheaded or faint, especially when standing up quickly.
Difficulty breathing, especially during physical activity or when lying down.
Fatigue: Unusual tiredness or weakness, even after rest.
Chest Pain: Pressure or discomfort in the chest, which can be a sign of cardiovascular strain.
It is important to note that some individuals with hyperparathyroidism and high blood pressure may not experience any symptoms, which is why regular blood pressure monitoring is essential for early detection and management.
Diagnosis of Hyperparathyroidism-Induced Hypertension
To diagnose hypertension in the context of hyperparathyroidism, a healthcare provider will perform a thorough medical evaluation, including:
Blood Tests: Blood tests will measure calcium levels, parathyroid hormone (PTH) levels, and kidney function. Elevated PTH levels and high calcium levels in the blood are indicative of hyperparathyroidism.
Imaging Tests: Ultrasound or nuclear scans may be used to identify abnormalities in the parathyroid glands, such as tumors or enlargement.
Blood Pressure Monitoring: Blood pressure will be monitored regularly to assess for hypertension. If blood pressure is consistently high, additional tests may be ordered to investigate the underlying cause.
Kidney Function Tests: Kidney function will be assessed, as impaired kidney function can contribute to the development of hypertension.
Treatment of Hypertension in Hyperparathyroidism
The treatment of hypertension caused by hyperparathyroidism focuses on addressing the underlying hyperparathyroidism and managing blood pressure. The following treatment strategies are commonly used:
Surgical Removal of Parathyroid Glands (Parathyroidectomy) The most effective treatment for primary hyperparathyroidism is the surgical removal of the overactive parathyroid gland(s). This procedure, known as a parathyroidectomy, can correct the calcium imbalance and reduce the elevated blood pressure associated with hyperparathyroidism. In cases of secondary hyperparathyroidism, the underlying cause (such as kidney disease) must also be addressed.
Medications to Lower Blood Pressure In addition to treating hyperparathyroidism, antihypertensive medications may be prescribed to control blood pressure. Common classes of medications used to treat hypertension include:
- Angiotensin-converting enzyme inhibitors (ACE inhibitors)
- Angiotensin II receptor blockers (ARBs)
- Calcium channel blockers
- Diuretics
Calcium and Vitamin D Management In patients with secondary hyperparathyroidism, calcium and vitamin D levels may be monitored and adjusted to help regulate PTH production. Proper management of calcium and vitamin D levels can help control blood pressure and prevent further complications.
Lifestyle Modifications Lifestyle changes can help manage both hypertension and hyperparathyroidism. These may include:
- Reducing salt intake
- Maintaining a healthy weight
- Engaging in regular physical activity
- Limiting alcohol consumption
- Quitting smoking
Conclusion
Hyperparathyroidism is a condition characterized by excessive production of parathyroid hormone, leading to elevated calcium levels in the blood. This imbalance can cause several cardiovascular complications, including hypertension. The mechanisms behind this include increased vascular resistance, enhanced sympathetic nervous system activity, kidney dysfunction, and activation of the renin-angiotensin-aldosterone system. Early diagnosis and treatment of hyperparathyroidism are crucial in preventing or managing hypertension and reducing the risk of cardiovascular damage.
Related topics: