Atrial flutter is a type of abnormal heart rhythm, or arrhythmia, that originates in the atria (the upper chambers of the heart). It is characterized by a rapid, organized rhythm, which is different from other arrhythmias like atrial fibrillation. In this article, we will explore the pathophysiology of atrial flutter, explaining the causes, the mechanisms behind it, and how it affects the heart.
Overview of Atrial Flutter
Atrial flutter is a type of supraventricular tachycardia (SVT), meaning that it originates above the ventricles in the atria. It is generally defined by a regular but fast heart rhythm, typically between 250 and 350 beats per minute. This rhythm is often seen in patients with underlying heart conditions but can also occur in those without any prior heart disease.
The hallmark of atrial flutter is a rapid, organized electrical impulse that is usually regular, with the atria contracting faster than the ventricles. This leads to an abnormal heart rate, which can have a variety of symptoms and complications, depending on its severity and duration.
Normal Electrical Conduction in the Heart
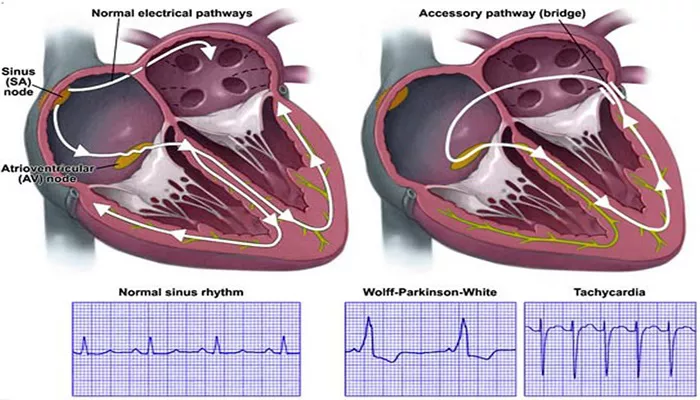
To understand atrial flutter, it’s important to first understand the normal electrical conduction system of the heart. The heart’s electrical system controls the heartbeat by sending electrical signals through the heart muscle. These signals help the heart beat in a coordinated and efficient way. The normal conduction pathway is as follows:
Sinoatrial (SA) Node: The SA node, located in the right atrium, generates electrical impulses that initiate each heartbeat.
It is known as the “natural pacemaker” of the heart.
Atria: The electrical signal spreads from the SA node through the atria, causing them to contract and push blood into the ventricles.
Atrioventricular (AV) Node: The electrical impulse travels through the AV node, which serves as a gatekeeper, slowing down the electrical signal before it reaches the ventricles.
His-Purkinje System: Finally, the electrical impulse travels down the bundle of His and the Purkinje fibers, causing the ventricles to contract and pump blood to the lungs and the rest of the body.
In a normal heart, this sequence occurs in a highly coordinated manner, resulting in a regular, normal heart rhythm.
Mechanism of Atrial Flutter
The pathophysiology of atrial flutter revolves around a specific type of abnormal electrical circuit in the atria. Unlike normal conduction, where the electrical impulses flow in one direction, atrial flutter involves a reentrant circuit. This reentry circuit causes the atria to beat very quickly and regularly. Let’s break down how this process works.
1. Reentrant Circuit in the Right Atrium
The most common form of atrial flutter involves a reentrant circuit in the right atrium. This circuit often follows a loop-like path around the tricuspid valve, creating a continuous electrical signal. The signal repeatedly travels through the right atrium in a circular manner, which leads to the rapid atrial contractions characteristic of atrial flutter.
In this circuit, electrical impulses continuously travel around the atria, causing the atria to contract rapidly, typically at rates of 250 to 350 beats per minute. However, not all of these impulses are able to pass through the AV node to the ventricles.
2. AV Node Role in Limiting Ventricular Rate
While the atria may be contracting at a very fast rate, the AV node plays an important role in limiting the number of electrical impulses that pass through to the ventricles. Normally, the AV node cannot transmit all the rapid signals from the atria to the ventricles. This results in a slower ventricular response, which can be anywhere from 120 to 150 beats per minute, depending on the severity of the flutter and the efficiency of the AV node.
The AV node acts as a filter, allowing only a portion of the electrical impulses to reach the ventricles. This is why atrial flutter is often associated with a ventricular rate that is lower than the atrial rate, but still faster than normal.
3. Effect of Atrial Flutter on Heart Function
Despite the AV node’s filtering role, the rapid atrial contractions in atrial flutter can still have significant effects on the heart’s overall function.
The rapid beating of the atria reduces the time available for the ventricles to fill with blood. This can lead to reduced cardiac output, especially if the flutter is sustained over a long period of time.
Additionally, the inefficient atrial contractions increase the risk of blood pooling and clot formation, especially in the left atrium. This is why atrial flutter, like atrial fibrillation, is associated with an increased risk of stroke and other complications.
Risk Factors for Atrial Flutter
Several factors can predispose a person to developing atrial flutter.
These include:
Heart Disease: Conditions such as coronary artery disease, heart failure, and valvular heart disease are among the most common causes of atrial flutter.
Hypertension: High blood pressure can lead to changes in the heart’s structure and electrical system, increasing the risk of arrhythmias.
Previous Heart Surgery: Individuals who have undergone heart surgery may develop scar tissue, which can alter the normal conduction pathways, leading to atrial flutter.
Electrolyte Imbalances: Imbalances in electrolytes such as potassium, magnesium, or calcium can disrupt the electrical activity of the heart.
Other Conditions: Hyperthyroidism, sleep apnea, and excessive alcohol consumption are also known to increase the risk of atrial flutter.
Symptoms of Atrial Flutter
The symptoms of atrial flutter can vary depending on the rate of the rhythm and whether the person has other heart conditions. Common symptoms include:
Palpitations: A feeling of a fast or irregular heartbeat.
Shortness of Breath: This occurs due to the reduced efficiency of the heart in pumping blood.
Fatigue: The rapid atrial rate can cause the heart to work less efficiently, leading to fatigue.
Dizziness or Lightheadedness: The decreased cardiac output and blood flow to the brain can cause these symptoms.
Chest Pain: Some individuals may experience chest discomfort or pain due to the strain on the heart.
Diagnosis of Atrial Flutter
Atrial flutter can be diagnosed through an electrocardiogram (ECG), which records the electrical activity of the heart. The characteristic findings of atrial flutter on an ECG include:
Sawtooth Waves: The atrial activity appears as a series of regular, sawtooth-like waves (known as F-waves), particularly in leads II, III, and aVF.
Regular Ventricular Response: The ventricular rate is usually regular but faster than normal, typically around 120 to 150 beats per minute.
No Distinct P Waves: Unlike in normal sinus rhythm, the P waves are absent or replaced by the sawtooth-like F-waves in atrial flutter.
Treatment Options for Atrial Flutter
The treatment of atrial flutter depends on the duration of the condition, the severity of symptoms, and the presence of underlying heart disease. Common treatment approaches include:
1. Rate Control
Rate control medications, such as beta-blockers or calcium channel blockers, are used to slow the ventricular rate. These medications help prevent the heart from beating too quickly, improving symptoms and reducing the risk of complications.
2. Rhythm Control
In some cases, restoring normal sinus rhythm (rhythm control) may be necessary. This can be done through medications such as antiarrhythmic drugs or electrical cardioversion, which delivers a shock to the heart to reset its electrical activity.
3. Ablation Therapy
For patients with recurrent or persistent atrial flutter, catheter ablation may be recommended. This procedure involves using radiofrequency energy to destroy the abnormal electrical pathways that cause the flutter.
4. Anticoagulation
Because atrial flutter increases the risk of blood clots, patients may be prescribed anticoagulant medications (blood thinners) to reduce the risk of stroke.
Conclusion
Atrial flutter is a common arrhythmia that involves a reentrant circuit in the atria, leading to rapid but organized atrial contractions. The condition can have a significant impact on heart function, causing symptoms like palpitations, shortness of breath, and fatigue. While the AV node filters the rapid atrial impulses, the ventricular rate remains elevated, and prolonged atrial flutter can increase the risk of stroke. Treatment strategies for atrial flutter include rate control, rhythm control, catheter ablation, and anticoagulation therapy, depending on the individual’s health status and the severity of the arrhythmia.
Related topics: