Atrial tachycardia is a type of arrhythmia, or abnormal heart rhythm, that originates in the upper chambers of the heart, known as the atria. In this condition, the heart beats faster than usual, and the electrical signals that control the heartbeat are disrupted. This can cause the heart to beat rapidly and irregularly, leading to symptoms such as palpitations, dizziness, shortness of breath, and in some cases, chest pain. Understanding how atrial tachycardia occurs is key to diagnosing and managing this condition effectively.
What Is Atrial Tachycardia?
Atrial tachycardia is a type of supraventricular tachycardia (SVT), which refers to any arrhythmia that originates above the ventricles in the heart’s electrical system. In atrial tachycardia, the electrical signals in the atria become abnormal, leading to a fast heart rate. The normal heart rate for an adult is typically between 60 and 100 beats per minute. However, in atrial tachycardia, the heart rate can increase to more than 100 beats per minute, and it can sometimes exceed 200 beats per minute.
The condition often occurs in episodes, which can last from a few seconds to several hours, and it can occur sporadically or more frequently depending on the individual.
The Heart’s Electrical System and Atrial Tachycardia
To understand how atrial tachycardia occurs, it’s important to know how the heart’s electrical system works. The heart has a natural pacemaker called the sinoatrial (SA) node, located in the right atrium.
The SA node generates electrical signals that initiate each heartbeat, causing the heart to contract and pump blood. These electrical signals travel through the atria and reach the atrioventricular (AV) node, which acts as a gatekeeper to control the flow of electrical impulses into the ventricles. The ventricles then contract and pump blood to the lungs and the rest of the body.
In a healthy heart, electrical signals flow in a controlled and coordinated manner, allowing the heart to beat in a steady rhythm.
However, in atrial tachycardia, the normal electrical impulses are disrupted, and additional electrical circuits or abnormal signals in the atria cause the heart to beat too quickly.
Causes of Atrial Tachycardia
Atrial tachycardia can result from a variety of factors that affect the heart’s electrical system. Some common causes include:
1. Structural Heart Disease
Conditions like heart disease, heart failure, or previous heart surgery can lead to changes in the structure of the heart.
These changes can disrupt the normal electrical pathways, causing abnormal signals to form and triggering atrial tachycardia.
2. Electrolyte Imbalance
Electrolytes, such as potassium, magnesium, and calcium, play a crucial role in the transmission of electrical signals in the heart. An imbalance of these electrolytes can lead to arrhythmias, including atrial tachycardia.
3. High Blood Pressure
Chronic high blood pressure (hypertension) can increase the workload on the heart and cause changes in the atria, leading to atrial tachycardia.
4. Heart Valve Disorders
Diseases of the heart valves, such as mitral valve prolapse or valve stenosis, can create turbulent blood flow in the heart.
This may result in the development of abnormal electrical circuits in the atria, leading to arrhythmias.
5. Congenital Heart Defects
Some individuals are born with structural abnormalities in the heart, which can increase the risk of developing atrial tachycardia.
6. Excessive Alcohol or Caffeine Consumption
Stimulants like alcohol, caffeine, and other drugs can increase the risk of arrhythmias by affecting the heart’s electrical system. In some cases, excessive consumption of these substances can trigger episodes of atrial tachycardia.
7. Thyroid Disorders
Conditions like hyperthyroidism, where the thyroid gland produces excess thyroid hormone, can speed up the metabolism and the heart rate, contributing to the development of atrial tachycardia.
8. Stress and Anxiety
Emotional stress or anxiety can trigger the release of stress hormones, which can affect the heart and lead to arrhythmias, including atrial tachycardia.
9. Sleep Apnea
Sleep apnea, a condition where breathing stops and starts during sleep, can lead to fluctuations in oxygen levels and an increased risk of atrial tachycardia.
Mechanism of Atrial Tachycardia
Atrial tachycardia occurs when an abnormal electrical signal is generated in the atria. The cause of these abnormal signals can be classified into two main mechanisms: automaticity and reentry.
1. Automaticity
In some cases, a single area of the atria becomes overactive and generates rapid electrical signals without the usual regulation from the SA node. This leads to an increased heart rate as the abnormal pacemaker cells take over control of the heart’s rhythm.
2. Reentry
Reentry occurs when an electrical signal travels in a circular loop, repeatedly stimulating the atria. This creates a rapid heart rate, as the signal keeps firing, causing the heart to beat faster than normal.
Both mechanisms lead to the abnormal conduction of electrical signals, which results in a rapid and irregular heart rhythm.
Symptoms of Atrial Tachycardia
Atrial tachycardia can present with a range of symptoms, which can vary in severity depending on the individual. Common symptoms include:
Palpitations: A sensation of a racing, fluttering, or irregular heartbeat.
Dizziness or lightheadedness: Due to reduced blood flow to the brain.
Shortness of breath: Difficulty breathing, especially during physical exertion.
Chest pain: A feeling of tightness or discomfort in the chest.
Fatigue: A feeling of extreme tiredness or weakness.
Fainting: In severe cases, the heart may not pump enough blood, leading to fainting.
Diagnosis of Atrial Tachycardia
If a person experiences symptoms of atrial tachycardia, a healthcare provider will perform several diagnostic tests to confirm the condition and determine its cause. These tests may include:
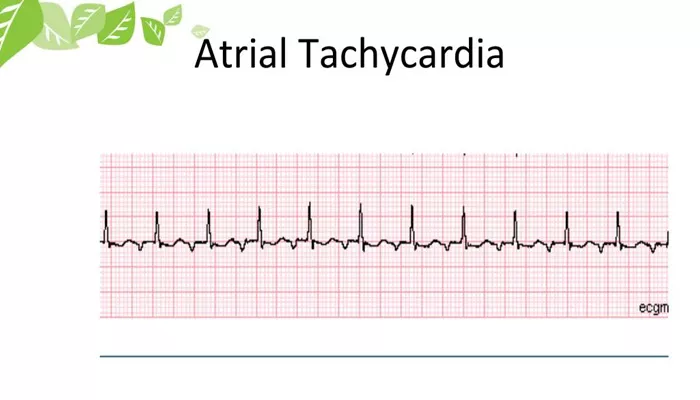
1. Electrocardiogram (ECG)
An ECG is the primary tool used to diagnose arrhythmias. It records the electrical activity of the heart and can reveal abnormal patterns associated with atrial tachycardia.
2. Holter Monitor
A Holter monitor is a portable ECG device that records the heart’s electrical activity over 24 to 48 hours. This test can help identify arrhythmias that occur intermittently.
3. Echocardiogram
An echocardiogram uses sound waves to create images of the heart’s structure and function. It can help detect any underlying heart disease that may be contributing to the arrhythmia.
4. Blood Tests
Blood tests can measure electrolyte levels, thyroid function, and other markers that may indicate an underlying cause of atrial tachycardia.
Treatment of Atrial Tachycardia
Treatment for atrial tachycardia depends on the severity of symptoms, the underlying cause, and the individual’s overall health. Some common treatment options include:
1. Medications
Antiarrhythmic drugs can be used to control the heart’s rhythm. Beta-blockers and calcium channel blockers may also be prescribed to slow the heart rate.
2. Cardioversion
If atrial tachycardia is causing severe symptoms, electrical cardioversion may be used to reset the heart’s rhythm. During this procedure, a controlled electric shock is delivered to the heart to restore a normal rhythm.
3. Catheter Ablation
In cases where medications are ineffective, catheter ablation may be performed. This procedure involves using a catheter to destroy the abnormal tissue causing the arrhythmia.
4. Lifestyle Modifications
Avoiding triggers such as excessive caffeine, alcohol, and stress can help manage atrial tachycardia. Managing underlying conditions like high blood pressure and sleep apnea is also important for prevention.
Conclusion
Atrial tachycardia occurs when abnormal electrical signals in the atria cause the heart to beat too quickly. It can be triggered by a variety of factors, including heart disease, electrolyte imbalances, and lifestyle choices. Recognizing the symptoms and understanding the underlying causes of atrial tachycardia are crucial for effective treatment and management. With proper care and intervention, most individuals with atrial tachycardia can lead healthy, active lives.
Related topics: