Supraventricular Tachycardia (SVT) is a type of abnormal heart rhythm that originates in the upper chambers of the heart, the atria. It is characterized by episodes of rapid heart rate, often over 100 beats per minute, which can lead to symptoms such as dizziness, shortness of breath, chest discomfort, and palpitations. SVT can happen unexpectedly and may even occur at night, which raises the question: Why does SVT happen more often at night? In this article, we will explore the reasons behind nighttime SVT episodes, potential triggers, and how it can be managed.
What Is SVT?
Before diving into the specific reasons why SVT may occur at night, it is important to understand what SVT is. SVT refers to any abnormal heart rhythm that begins in the atria or the atrioventricular (AV) node. There are different types of SVT, including atrial fibrillation, atrial flutter, and paroxysmal SVT, each with its own set of causes and symptoms.
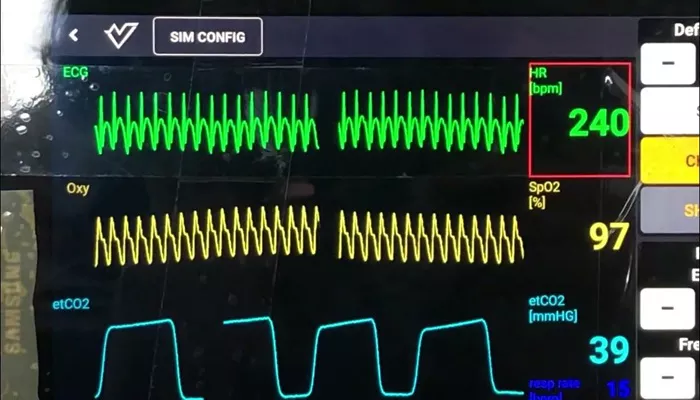
SVT episodes occur when there is a disruption in the normal electrical pathways of the heart, leading to a rapid and irregular heart rate. These episodes can start suddenly and may last for a few seconds, minutes, or even hours. They are often triggered by external factors like stress, caffeine, alcohol, or certain medications, and they can sometimes happen without any clear trigger.
Why Does SVT Occur at Night?
While SVT can occur at any time, many individuals report that they experience episodes more frequently during the night or when they are trying to fall asleep. There are several possible reasons for this:
Changes in Autonomic Nervous System Activity at Night
The autonomic nervous system (ANS) regulates involuntary functions in the body, including heart rate and blood pressure.
The ANS has two main components: the sympathetic nervous system (which activates the “fight or flight” response) and the parasympathetic nervous system (which promotes relaxation and recovery).
At night, the body enters a more relaxed state, and the parasympathetic nervous system becomes more dominant. This shift can cause a drop in heart rate and blood pressure. However, in some individuals with SVT, this parasympathetic dominance can trigger an episode by altering the electrical activity in the heart. In particular, increased vagal tone (a parasympathetic response) can lead to the initiation of abnormal heart rhythms, including SVT.
Lying Down and Increased Blood Flow to the Heart
When you lie down, especially after a long day of standing or sitting, the body’s blood flow and circulation change. Blood returns more easily to the heart, which can affect the electrical impulses that control the heart’s rhythm. In some cases, this change in blood flow can trigger an SVT episode. The heart may respond to this increased blood return by firing off electrical signals too rapidly, leading to a faster-than-normal heart rate.
Decreased Distractions and Stress Levels at Night
During the day, you may experience a higher level of physical and emotional activity, which can act as distractions from any underlying heart issues. At night, however, when the body is at rest and the mind is quiet, you may become more aware of your heart rate and any irregularities in it. Additionally, at night, the stress and anxiety of the day may also subside, leading to a shift in autonomic control, which can contribute to an episode of SVT.
Hormonal Fluctuations
Hormonal changes throughout the day can influence your heart rate and overall cardiovascular function. These changes may be more prominent at night, particularly in relation to the natural circadian rhythms of your body. Some individuals with SVT may find that their episodes are more likely to occur during specific hormonal cycles or in response to fluctuations in their body’s natural rhythms. This is especially true for women, as hormonal changes related to menstruation, pregnancy, and menopause can impact the frequency and intensity of SVT episodes.
Sleep Apnea and Other Sleep Disorders
Sleep apnea is a condition where a person’s breathing repeatedly stops and starts during sleep. This can cause fluctuations in oxygen levels and increases in heart rate, leading to stress on the heart. For some individuals with SVT, sleep apnea may trigger episodes of rapid heart rate. People who are overweight, have high blood pressure, or suffer from other heart conditions may be at an increased risk of both sleep apnea and SVT.
Medications Taken at Night
Some individuals with SVT may take medications before bedtime to help control the condition or manage symptoms.
Certain medications, such as beta-blockers or anti-arrhythmic drugs, may alter heart function in ways that make it more likely to experience SVT during the night. Additionally, other substances such as alcohol, caffeine, or nicotine, consumed before bed, can also increase the likelihood of SVT episodes.
How to Manage SVT Episodes at Night
Managing SVT episodes, particularly those that occur at night, involves a combination of lifestyle adjustments and medical treatments. If you experience frequent or prolonged SVT episodes at night, it is important to discuss these with your healthcare provider. Below are some strategies to help manage nighttime SVT:
Establish a Consistent Sleep Routine
Maintaining a regular sleep schedule can help regulate the autonomic nervous system and reduce the chances of SVT episodes occurring during the night. Try to go to bed and wake up at the same time each day, and make sure your sleeping environment is conducive to relaxation and rest.
Avoid Stimulants Before Bed
Caffeine, nicotine, and alcohol can all trigger SVT episodes. Try to avoid these substances in the hours leading up to bedtime. Limiting screen time before bed can also help reduce the risk of overstimulation that may affect sleep and heart rate.
Monitor and Manage Stress
Stress is a known trigger for SVT. Practicing relaxation techniques such as deep breathing, meditation, or progressive muscle relaxation can help calm your mind and body before sleep, potentially preventing SVT episodes from occurring.
Address Sleep Apnea
If sleep apnea is a concern, it is important to seek appropriate treatment. Continuous positive airway pressure (CPAP) therapy is often used to manage sleep apnea and may help reduce the frequency of SVT episodes. Your doctor may also recommend lifestyle changes such as weight loss or sleeping on your side.
Medication and Medical Treatments
If your SVT episodes persist despite lifestyle modifications, medications or procedures may be necessary. Your healthcare provider may recommend anti-arrhythmic drugs, beta-blockers, or other treatments to help regulate your heart rhythm. In some cases, a procedure called catheter ablation may be recommended to correct abnormal electrical pathways in the heart.
Conclusion
While SVT episodes at night can be unsettling, understanding the factors that contribute to these events can help individuals better manage and prevent them. The shift in autonomic nervous system activity, changes in blood flow, hormonal fluctuations, and even sleep disorders can all play a role in triggering SVT during sleep. By implementing lifestyle changes and working closely with your healthcare provider, you can take steps to reduce the frequency and severity of nighttime SVT episodes and improve your overall heart health.
Related topics: