Ventricular tachycardia (VT) is a type of arrhythmia or irregular heartbeat that originates in the lower chambers of the heart, called the ventricles. This condition occurs when the electrical signals that regulate the heart’s rhythm become abnormal, leading to a rapid heartbeat. The ventricles typically pump blood to the body, and when they beat too fast or irregularly, it can affect the heart’s ability to pump blood effectively.
VT is often a serious condition that can lead to life-threatening complications, including sudden cardiac arrest. It is important for both patients and healthcare providers to understand the causes, symptoms, diagnosis, and treatment options for this arrhythmia.
What Happens During Ventricular Tachycardia?
The heart has a natural pacemaker called the sinoatrial (SA) node that sends electrical signals to the atria (the upper chambers of the heart). These signals then travel through a network of specialized pathways to the ventricles, instructing them when to contract and pump blood. In VT, the electrical signals in the ventricles become disordered and cause the ventricles to beat much faster than normal. This rapid heart rate can range from 100 to 250 beats per minute, which is much higher than the normal resting heart rate of 60 to 100 beats per minute.
As the ventricles beat too quickly, they don’t have enough time to fill with blood between beats. This decreases the amount of blood that is pumped to the rest of the body, leading to reduced oxygen supply for the organs, including the brain. This can result in dizziness, fainting, and, if left untreated, even sudden cardiac arrest.
Types of Ventricular Tachycardia
There are two main types of ventricular tachycardia:
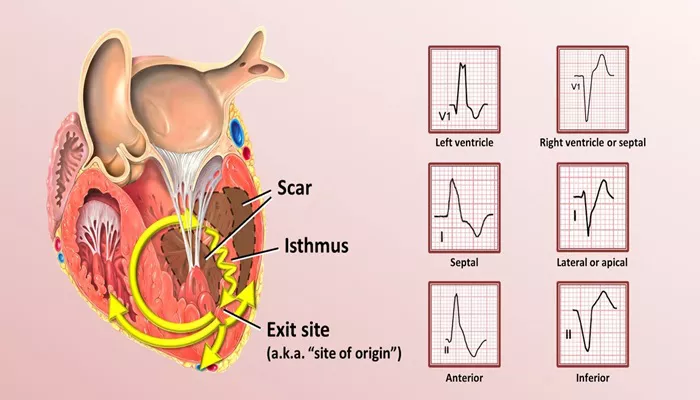
Monomorphic Ventricular Tachycardia: In this type, the shape and rhythm of the electrical signals are consistent. The abnormal electrical impulses come from the same point in the ventricles, and the heartbeats have a uniform pattern.
Polymorphic Ventricular Tachycardia: In this type, the electrical signals are irregular and originate from different areas of the ventricles. The heartbeats can appear in varying shapes and patterns, making this type of VT more unpredictable and dangerous. One well-known form of polymorphic VT is called Torsades de Pointes, which is often associated with a prolonged QT interval on an electrocardiogram (ECG).
Causes of Ventricular Tachycardia
Ventricular tachycardia can be triggered by a variety of underlying conditions. Some of the most common causes include:
Coronary Artery Disease (CAD): CAD occurs when the blood vessels that supply the heart muscle become narrowed or blocked, reducing blood flow. This can lead to damage to the heart muscle and increase the risk of VT.
Heart Attack (Myocardial Infarction): A heart attack can cause scarring of the heart muscle, disrupting normal electrical signals and leading to VT.
Heart Failure: When the heart becomes weakened and cannot pump blood effectively, the risk of arrhythmias, including VT, increases.
Cardiomyopathy: This condition refers to diseases of the heart muscle, which can lead to abnormal heart rhythms, including VT.
Electrolyte Imbalances: Abnormal levels of electrolytes such as potassium, magnesium, or calcium can affect the heart’s electrical system and trigger VT.
Inherited Conditions: Certain genetic conditions, such as Long QT Syndrome or Brugada Syndrome, can predispose individuals to VT.
Drug Use: Certain medications or drugs, such as those that prolong the QT interval or cause heart rhythm disturbances, can trigger VT.
Other Heart Conditions: Conditions like valve disease or congenital heart defects can also increase the risk of developing VT.
Symptoms of Ventricular Tachycardia
The symptoms of VT can vary depending on the severity and duration of the arrhythmia. Some individuals may experience no symptoms, while others may experience:
Palpitations: A sensation of a rapid or irregular heartbeat.
Dizziness or Lightheadedness: Reduced blood flow to the brain can lead to feelings of dizziness or even fainting.
Chest Pain or Discomfort: Some individuals may feel pressure or tightness in the chest.
Shortness of Breath: Difficulty breathing or a feeling of breathlessness can occur as the heart struggles to pump blood effectively.
Fainting (Syncope): Sudden, brief loss of consciousness due to reduced blood flow to the brain is a common symptom of VT.
Cardiac Arrest: In severe cases, VT can progress to ventricular fibrillation, a life-threatening arrhythmia that leads to sudden cardiac arrest.
Diagnosis of Ventricular Tachycardia
To diagnose VT, healthcare providers rely on several tools:
Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart. A typical finding in VT is a rapid, irregular rhythm originating from the ventricles.
Holter Monitor: This is a portable ECG that records heart activity over 24 to 48 hours to capture any abnormal rhythms that may not appear during a routine ECG.
Echocardiogram: An ultrasound of the heart that can help detect structural problems or damage to the heart muscle that may be causing VT.
Electrophysiological Study (EPS): This invasive procedure involves inserting a catheter into the heart to map the electrical signals and pinpoint the source of the arrhythmia.
Cardiac MRI or CT Scan: In some cases, imaging techniques may be used to evaluate the heart’s structure and identify any underlying issues.
Treatment of Ventricular Tachycardia
The treatment of VT depends on the severity of the condition, the underlying cause, and the symptoms the patient is experiencing. Some common treatments include:
Medications: Antiarrhythmic drugs such as amiodarone, sotalol, or lidocaine can help control VT by stabilizing the heart’s electrical activity. Beta-blockers may also be used to reduce the frequency of episodes.
Cardioversion: This is a procedure in which a controlled electrical shock is delivered to the heart to reset the rhythm. It is typically used when VT is causing significant symptoms or when other treatments have not worked.
Implantable Cardioverter-Defibrillator (ICD): An ICD is a small device implanted under the skin that monitors the heart’s rhythm. If it detects VT or other life-threatening arrhythmias, it delivers an electrical shock to restore normal rhythm.
Catheter Ablation: In cases where VT is caused by a specific area of abnormal electrical activity, a catheter ablation may be performed. During this procedure, a catheter is used to destroy the tissue responsible for the arrhythmia.
Lifestyle Changes: Managing underlying conditions such as high blood pressure, diabetes, or high cholesterol is important for preventing VT. Regular exercise, a heart-healthy diet, and avoiding smoking and excessive alcohol can also help reduce the risk.
Surgery: In rare cases, surgery may be required to repair structural issues in the heart that are contributing to VT.
Prevention of Ventricular Tachycardia
While not all cases of VT can be prevented, individuals can take steps to reduce their risk:
Manage Heart Disease: Properly managing conditions like coronary artery disease, heart failure, and cardiomyopathy can lower the likelihood of developing VT.
Regular Check-ups: Individuals with a history of heart disease should have regular check-ups with their healthcare provider to monitor their heart’s health.
Avoid Triggers: Avoiding substances that can trigger arrhythmias, such as stimulants (e.g., caffeine or drugs) or medications that may affect heart rhythm, is important.
Know the Signs: Understanding the symptoms of VT and seeking medical attention promptly can help reduce the risk of complications.
Conclusion
Ventricular tachycardia is a potentially life-threatening arrhythmia that can have serious consequences if not treated promptly. Understanding its causes, symptoms, and treatment options is essential for individuals at risk. Early diagnosis and appropriate management are key to preventing complications, including sudden cardiac arrest. With advances in medical technology, individuals with VT can often lead normal, active lives by working closely with their healthcare providers to manage the condition effectively.
Related topics: