Atrial flutter is a type of abnormal heart rhythm (arrhythmia) that originates in the heart’s upper chambers, known as the atria. This condition involves rapid and regular heartbeats, and it can cause symptoms like palpitations, dizziness, shortness of breath, and fatigue. Understanding atrial flutter is essential because it can lead to serious complications, such as stroke or heart failure, if left untreated. In this article, we will explore the causes, symptoms, diagnosis, and treatment options for atrial flutter.
The Basics of Atrial Flutter
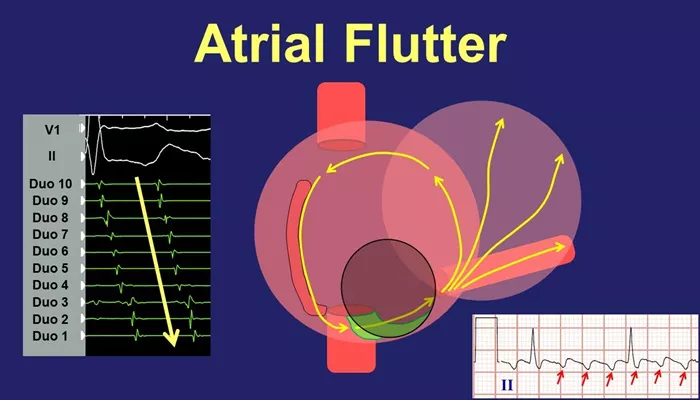
Atrial flutter is characterized by an abnormal electrical signal in the heart’s atria. The electrical impulses in the atria fire at a much higher rate than normal, often ranging from 250 to 350 beats per minute. However, not all of these impulses are conducted to the ventricles (the heart’s lower chambers), which means that the heart’s overall rhythm is faster than usual but not as high as the atrial rate.
In a healthy heart, electrical impulses travel from the atria to the ventricles in an orderly manner, leading to a normal rhythm. However, in atrial flutter, the electrical signals in the atria loop around in a circuit, causing the atria to beat rapidly and irregularly. This can lead to a decrease in the heart’s efficiency and may cause a variety of symptoms.
Causes of Atrial Flutter
Atrial flutter can be triggered by several factors, which include:
Heart Disease: Conditions such as coronary artery disease, heart failure, and high blood pressure can lead to changes in the heart’s electrical system, increasing the likelihood of atrial flutter.
Previous Heart Surgery: Individuals who have undergone heart surgery may be at a higher risk due to scarring or changes in the heart’s structure.
Valve Problems: Diseases affecting the heart valves, such as mitral valve disease, can cause atrial flutter by altering blood flow and heart pressure.
Hyperthyroidism: An overactive thyroid gland can increase the heart rate, contributing to the development of atrial flutter.
Pulmonary Conditions: Diseases such as chronic obstructive pulmonary disease (COPD) or pneumonia can also increase the risk.
Excessive Alcohol Consumption: Known as “holiday heart syndrome,” drinking large amounts of alcohol can trigger atrial flutter.
Electrolyte Imbalances: Low levels of potassium or magnesium can disrupt the heart’s electrical signals, leading to arrhythmias like atrial flutter.
Genetic Predisposition: Family history of arrhythmias may also play a role in the development of atrial flutter.
Symptoms of Atrial Flutter
Atrial flutter does not always cause noticeable symptoms, but when symptoms do occur, they can include:
Palpitations: A fluttering or racing feeling in the chest.
Shortness of Breath: Difficulty breathing or feeling winded even with mild exertion.
Fatigue: Unusual tiredness or weakness, especially after physical activity.
Dizziness or Fainting: A sensation of lightheadedness or even fainting, which can occur if the heart is not pumping blood effectively.
Chest Pain: In some cases, chest discomfort or pain can occur, especially if the atrial flutter is related to underlying heart disease.
Potential Complications of Atrial Flutter
Although atrial flutter itself is not usually life-threatening, it can lead to several serious complications:
Stroke: The rapid and irregular heart rhythm in atrial flutter increases the risk of blood clots forming in the atria. These clots can travel to the brain, leading to a stroke.
Heart Failure: If left untreated, atrial flutter can cause the heart to pump inefficiently, leading to heart failure over time.
Reduced Quality of Life: The symptoms of atrial flutter, such as palpitations, fatigue, and dizziness, can interfere with daily activities and reduce a person’s quality of life.
How Is Atrial Flutter Diagnosed?
Diagnosing atrial flutter typically involves a few steps:
1. Physical Examination
A doctor will begin by asking about the patient’s symptoms and medical history. During the physical exam, the doctor will listen to the heart with a stethoscope and check for irregularities in the heart’s rhythm.
2. Electrocardiogram (ECG or EKG)
An electrocardiogram is the primary tool used to diagnose atrial flutter.
This test records the electrical activity of the heart and can reveal the characteristic “sawtooth” pattern of atrial flutter waves. An ECG can also help differentiate atrial flutter from other types of arrhythmias, such as atrial fibrillation.
3. Holter Monitor
In some cases, a doctor may recommend wearing a Holter monitor, a portable device that records the heart’s electrical activity over 24 to 48 hours. This can help identify intermittent episodes of atrial flutter that may not be detected during a regular ECG.
4. Electrophysiological Study (EPS)
An electrophysiological study is a procedure where catheters are inserted into the heart to map its electrical activity. This test is usually performed if the patient’s arrhythmia is difficult to diagnose or if more information is needed to guide treatment.
Treatment of Atrial Flutter
Treating atrial flutter involves both managing symptoms and addressing the underlying causes of the condition. The primary goals of treatment are to restore a normal heart rhythm and prevent complications such as stroke or heart failure.
Treatment options include medications, electrical procedures, and lifestyle changes.
1. Medications
Medications can be used to control the heart rate, restore a normal rhythm, or prevent blood clots. These include:
Beta-Blockers: These medications help slow the heart rate and reduce the symptoms of atrial flutter.
Calcium Channel Blockers: These drugs can also help control the heart rate by blocking calcium channels in the heart.
Antiarrhythmic Drugs: These medications help restore a normal heart rhythm and prevent future episodes of atrial flutter.
Anticoagulants: Because atrial flutter increases the risk of blood clots, patients may be prescribed blood thinners to prevent stroke.
2. Electrical Cardioversion
Electrical cardioversion is a procedure where a controlled shock is delivered to the heart to restore a normal rhythm. This is often used when medications are ineffective or when the patient is experiencing severe symptoms.
3. Catheter Ablation
Catheter ablation is a procedure used to treat atrial flutter in patients who do not respond well to medications or electrical cardioversion. It involves threading a catheter through blood vessels to the heart, where it delivers radiofrequency energy to destroy the abnormal electrical pathways causing the arrhythmia. This treatment has a high success rate and can offer a long-term solution for many patients.
4. Lifestyle Changes
Certain lifestyle changes can help manage atrial flutter, particularly when it is triggered by external factors such as alcohol or excessive stress. These changes may include:
Limiting Alcohol Consumption: Reducing alcohol intake may help prevent episodes of atrial flutter.
Managing Stress: Techniques such as relaxation exercises, yoga, or meditation can help reduce stress, which may trigger arrhythmias.
Eating a Healthy Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins can improve overall heart health and reduce the risk of arrhythmias.
Conclusion
Atrial flutter is a type of arrhythmia that can cause rapid heartbeats and lead to significant health problems, such as stroke and heart failure, if not properly managed. Understanding the causes, symptoms, and treatment options for atrial flutter is essential in preventing complications and improving the quality of life for individuals affected by this condition. If you suspect you have atrial flutter or have been diagnosed with it, work closely with your healthcare provider to develop a personalized treatment plan and stay informed about ways to manage the condition effectively.
Related topics: