Supraventricular Tachycardia (SVT) is a condition that causes a rapid heart rate, originating above the heart’s ventricles.
This condition is often associated with irregular heartbeats and can lead to significant symptoms, ranging from mild discomfort to more severe complications. Understanding SVT is essential for early diagnosis, appropriate management, and effective treatment. In this article, we will explore the nature of SVT, its causes, symptoms, diagnosis, treatment options, and the overall outlook for individuals living with the condition.
Introduction to Supraventricular Tachycardia
Supraventricular Tachycardia refers to a group of heart rhythm disorders (arrhythmias) that originate in the upper chambers of the heart, known as the atria or the atrioventricular (AV) node. These conditions are characterized by episodes of abnormally fast heartbeats, often exceeding 100 beats per minute (bpm), and they typically occur suddenly.
SVT can affect people of all ages, but it is most commonly observed in young, healthy individuals. While SVT episodes are generally not life-threatening, they can cause significant discomfort and disrupt daily life. In some cases, if left untreated, SVT may lead to more severe heart problems. Fortunately, with proper medical care and lifestyle management, SVT can often be controlled and treated successfully.
The Normal Heart Rhythm
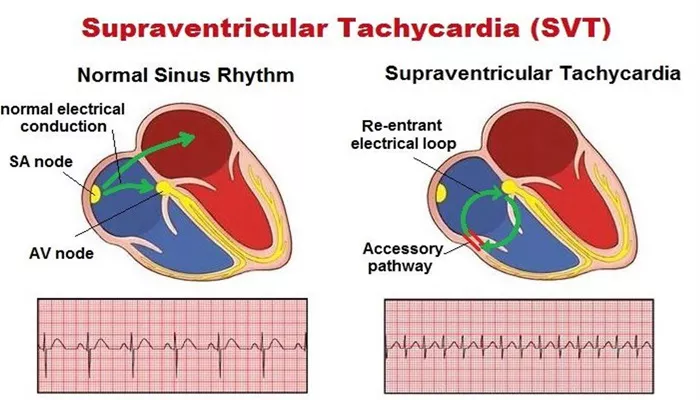
To understand what happens during an episode of SVT, it’s important first to look at how the heart typically functions. The heart is a muscle with four chambers: two atria (upper chambers) and two ventricles (lower chambers). Electrical impulses, generated by the sinoatrial (SA) node, control the heart’s rhythm, triggering the contraction of the atria and ventricles in a coordinated manner.
Under normal conditions, the heart rate ranges from 60 to 100 beats per minute, depending on factors like activity level, age, and physical condition. The electrical signals travel from the SA node to the AV node and then to the ventricles, ensuring that the heart beats in a steady, synchronized pattern. This coordinated rhythm allows the heart to efficiently pump blood throughout the body.
Causes of Supraventricular Tachycardia
SVT can be triggered by various factors, including congenital heart conditions, lifestyle choices, and external influences. In many cases, the exact cause remains unknown, but several common factors are associated with the development of SVT.
1. Abnormalities in the Electrical Pathways
SVT often results from abnormal electrical pathways in the heart.
These pathways can be congenital (present at birth) or develop later in life due to changes in the heart’s structure or function. Some common electrical issues include:
Accessory pathways: Extra electrical pathways in the heart, such as in Wolff-Parkinson-White (WPW) syndrome, can cause the heart to beat irregularly. These pathways bypass the AV node and allow the electrical impulses to travel too quickly, resulting in rapid heartbeats.
AV nodal reentrant tachycardia (AVNRT): This is one of the most common types of SVT and occurs when there is an abnormal circuit within the AV node itself, causing rapid heartbeats.
2. Heart Disease
Certain heart conditions can increase the risk of developing SVT.
These include:
Coronary artery disease: Blockages in the coronary arteries can affect the heart’s electrical system and may lead to arrhythmias such as SVT.
Heart failure: When the heart is weakened, it can result in electrical disturbances that contribute to the development of arrhythmias.
3. Lifestyle Factors
Lifestyle choices and external factors can trigger or exacerbate SVT.
These include:
Excessive caffeine or alcohol consumption: Stimulants like caffeine and alcohol can alter the heart’s electrical signals, triggering episodes of SVT.
Stress and anxiety: Emotional stress can increase the production of stress hormones such as adrenaline, which may lead to irregular heart rhythms.
Exercise: While physical activity generally supports heart health, intense or prolonged exercise can sometimes trigger SVT episodes, especially in individuals predisposed to arrhythmias.
4. Other Medical Conditions
Several medical conditions are associated with an increased risk of SVT, including:
Hyperthyroidism: Overactive thyroid glands can cause the heart to beat faster than normal.
Electrolyte imbalances: Low levels of potassium or magnesium can affect the electrical activity of the heart and increase the likelihood of arrhythmias.
Sleep apnea: Interrupted breathing during sleep can lead to fluctuations in heart rate, contributing to the development of SVT.
Symptoms of Supraventricular Tachycardia
The symptoms of SVT can vary from person to person. Some individuals may experience only mild discomfort during episodes, while others may have more severe symptoms. The most common symptoms include:
Rapid heart rate: One of the hallmark symptoms of SVT is a sudden increase in heart rate, often exceeding 150 beats per minute.
Palpitations: A sensation of a pounding or fluttering heartbeat.
Dizziness or lightheadedness: The rapid heart rate can reduce the heart’s efficiency, leading to insufficient blood flow to the brain, which may cause dizziness.
Shortness of breath: A fast heart rate can make it harder for the heart to pump blood effectively, leading to shortness of breath.
Chest pain: Some individuals with SVT may experience chest discomfort or pain, particularly if the condition leads to a decrease in oxygen supply to the heart muscle.
Fatigue: The increased workload on the heart during SVT episodes can lead to general tiredness or fatigue.
In some cases, SVT may not cause noticeable symptoms, especially if the episodes are brief and infrequent. However, when symptoms occur, they can significantly impact a person’s daily activities and quality of life.
Diagnosis of Supraventricular Tachycardia
Diagnosing SVT typically involves a combination of a detailed medical history, physical examination, and diagnostic tests.
Some of the most common methods for diagnosing SVT include:
1. Electrocardiogram (ECG)
An ECG is one of the most important tools for diagnosing SVT. This test records the electrical activity of the heart, allowing doctors to identify the specific type of arrhythmia and determine the origin of the rapid heart rate.
2. Holter Monitor
A Holter monitor is a portable ECG device worn by the patient for 24 to 48 hours. It continuously records the heart’s activity, helping doctors identify episodes of SVT that may not be detectable during a routine office visit.
3. Electrophysiology Study (EPS)
In cases where the diagnosis is unclear or treatment options need to be refined, doctors may perform an electrophysiology study. This test involves inserting catheters into the heart to map its electrical activity and locate abnormal pathways.
4. Blood Tests
Blood tests may be conducted to rule out underlying conditions, such as electrolyte imbalances or thyroid problems, that may contribute to SVT.
Treatment Options for Supraventricular Tachycardia
Although SVT is often not life-threatening, it requires proper management to reduce symptoms and prevent complications.
The treatment approach for SVT depends on the frequency and severity of episodes, as well as the underlying causes.
1. Vagal Maneuvers
For individuals experiencing an episode of SVT, certain vagal maneuvers can help slow the heart rate. These maneuvers stimulate the vagus nerve, which can help regulate the heart’s electrical activity. Common maneuvers include:
Valsalva maneuver: This involves bearing down, as though having a bowel movement, to increase pressure in the chest and stimulate the vagus nerve.
Coughing: Coughing forcefully can sometimes slow the heart rate.
Splashing cold water on the face: This can stimulate the vagus nerve and help slow down the heart rate.
2. Medications
Beta-blockers: These medications help slow the heart rate and reduce the frequency of SVT episodes.
Calcium channel blockers: These can also help control the heart rate and are often used for long-term management of SVT.
Antiarrhythmic drugs: In some cases, doctors may prescribe medications to regulate the heart’s rhythm and prevent episodes of SVT.
3. Catheter Ablation
For individuals with frequent or severe episodes of SVT that do not respond to medications, catheter ablation may be recommended. During this procedure, a catheter is inserted into the heart to destroy the abnormal electrical pathways responsible for the arrhythmia.
4. Surgery
In rare cases, when other treatments are not effective, surgery may be considered to remove or correct the abnormal electrical pathways in the heart.
Conclusion
Supraventricular Tachycardia is a relatively common but manageable condition that affects the heart’s rhythm. While SVT can cause distressing symptoms, with appropriate medical intervention, most individuals can manage their condition effectively. Understanding the causes, symptoms, and treatment options is key to living with SVT and maintaining overall heart health. If you experience symptoms of SVT, it is essential to consult a healthcare provider for proper evaluation and treatment.
Related topics: