Ventricular fibrillation (VF) is a life-threatening heart condition that occurs when the electrical activity of the heart becomes chaotic. This condition causes the heart’s lower chambers (ventricles) to quiver instead of contracting normally, leading to a rapid and ineffective heart rhythm. Ventricular fibrillation can result in sudden cardiac arrest, which requires immediate medical intervention to prevent death.
In this article, we will explore what ventricular fibrillation is, its causes, symptoms, diagnosis, treatment methods, and preventive measures. We aim to provide a clear, comprehensive understanding of this serious heart condition.
What Is Ventricular Fibrillation?
Ventricular fibrillation is a severe arrhythmia (irregular heart rhythm) that arises from the ventricles of the heart. The ventricles are the heart’s pumping chambers, and their primary function is to pump blood to the lungs and the rest of the body. In VF, the electrical impulses in the ventricles become disordered, preventing the heart from pumping blood effectively.
Unlike normal heartbeats, which follow a regular electrical pattern, the electrical signals in the ventricles during VF are rapid and erratic. This causes the heart to lose its ability to contract properly, and blood flow to the rest of the body comes to a halt. VF is the most common cause of sudden cardiac arrest, and if not treated immediately, it can result in death within minutes.
Causes of Ventricular Fibrillation
Ventricular fibrillation can be caused by a variety of factors, most of which are related to an underlying heart condition or damage to the heart muscle. The most common causes of VF include:
1. Coronary Artery Disease (CAD)
Coronary artery disease, a condition where the blood vessels supplying the heart with oxygen-rich blood become narrowed or blocked, is the most common cause of VF. When blood flow to the heart muscle is disrupted, it can lead to tissue damage, which increases the risk of developing VF.
2. Heart Attack (Myocardial Infarction)
A heart attack, also known as a myocardial infarction, occurs when the blood flow to part of the heart muscle is completely blocked. This lack of oxygen to the heart muscle can trigger an arrhythmia, including ventricular fibrillation.
3. Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle, which can become enlarged, thickened, or rigid. This can impair the heart’s ability to pump blood and increase the risk of developing VF, especially in the later stages of the condition.
4. Electrolyte Imbalances
Electrolytes, such as potassium, sodium, and calcium, are essential for the electrical conduction of the heart. An imbalance in these electrolytes can disrupt the heart’s electrical activity, potentially leading to VF.
5. Arrhythmogenic Right Ventricular Dysplasia (ARVD)
This is a rare genetic condition in which the tissue of the right ventricle becomes replaced with fatty or fibrous tissue. It can lead to abnormal electrical conduction and increase the risk of VF, especially in younger individuals.
6. Long QT Syndrome
Long QT syndrome is a disorder of the heart’s electrical system that causes the heart to take longer than usual to recharge between beats.
This condition can lead to abnormal heart rhythms, including VF.
7. Drug Use
Certain medications and illicit drugs, such as cocaine, can trigger VF by affecting the electrical activity of the heart.
Overdoses of these substances can significantly increase the risk of arrhythmias, including VF.
8. Other Conditions
Other medical conditions, including severe blood loss, trauma, and certain infections affecting the heart, can also contribute to the development of ventricular fibrillation.
Symptoms of Ventricular Fibrillation
Ventricular fibrillation develops suddenly and progresses rapidly. The symptoms of VF are directly related to the inability of the heart to pump blood effectively, leading to a sudden drop in blood pressure and oxygen levels in the body.
Common symptoms of VF include:
1. Sudden Loss of Consciousness
One of the first signs of VF is the sudden loss of consciousness. Without proper blood flow to the brain, a person will collapse and lose consciousness almost immediately.
2. Severe Chest Pain
Many individuals with VF experience severe chest pain before the onset of the arrhythmia. This is often a result of an underlying heart attack or coronary artery disease.
3. Rapid and Irregular Heartbeat
People experiencing VF may feel their heart racing or beating erratically, though this sensation may not be present before the person loses consciousness.
4. Shortness of Breath
Due to inadequate blood circulation, individuals with VF may struggle to breathe or experience a feeling of breathlessness.
5. Dizziness or Lightheadedness
A sudden drop in blood pressure can cause dizziness or lightheadedness, especially in the early stages of VF.
6. Sweating
Excessive sweating can occur as a result of the heart’s inability to pump blood efficiently during VF.
7. Pale or Cyanotic Skin
As blood flow decreases, the skin may become pale or develop a bluish tint, indicating that the tissues are not receiving enough oxygen.
If ventricular fibrillation is not treated immediately, the person will collapse and die due to a lack of oxygenated blood reaching vital organs like the brain and heart.
Diagnosis of Ventricular Fibrillation
The diagnosis of ventricular fibrillation is often made based on clinical symptoms and the results of several diagnostic tests.
Since VF causes a sudden loss of consciousness and collapse, it is typically diagnosed in an emergency setting.
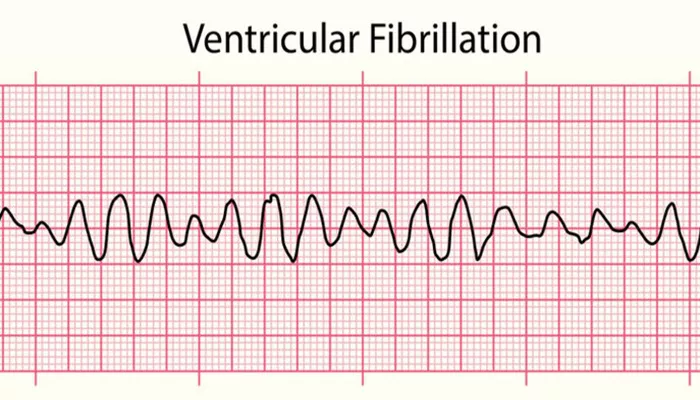
1. Electrocardiogram (ECG)
An electrocardiogram is the primary diagnostic tool for confirming VF. During an ECG, electrodes are placed on the chest to measure the electrical activity of the heart. In VF, the ECG will show a rapid, erratic rhythm with no clear pattern or recognizable heartbeats.
2. Physical Exam
Although VF is usually diagnosed through an ECG, healthcare providers may perform a physical exam to assess signs of cardiovascular collapse, such as a weak or absent pulse, low blood pressure, and abnormal breathing.
3. Blood Tests
Blood tests may be done to check for signs of a heart attack, electrolyte imbalances, or other factors that could contribute to the development of VF.
4. Imaging Tests
In some cases, imaging tests like echocardiograms or coronary angiograms may be performed to assess the underlying heart structure and identify conditions such as coronary artery disease or cardiomyopathy that may have triggered the VF.
Treatment of Ventricular Fibrillation
Ventricular fibrillation is a medical emergency that requires immediate treatment to restore a normal heart rhythm and prevent death. The main treatment for VF is defibrillation, which is the process of delivering a high-energy shock to the heart to reset its electrical activity.
1. Defibrillation
The most effective treatment for ventricular fibrillation is defibrillation, which is typically performed with an automated external defibrillator (AED) or a manual defibrillator. This device delivers a shock to the heart to stop the erratic electrical activity and allow the heart to resume normal rhythm. In cases of sudden cardiac arrest, defibrillation must occur within minutes to prevent death.
2. Cardiopulmonary Resuscitation (CPR)
While waiting for a defibrillator, performing CPR can help maintain circulation and oxygen flow to the brain and other vital organs. High-quality chest compressions are essential for improving the chances of survival in individuals experiencing VF.
3. Medications
In some cases, medications may be used to stabilize the heart and prevent further arrhythmias. Drugs such as amiodarone, lidocaine, or epinephrine may be administered to restore normal rhythm or manage complications.
4. Implantable Cardioverter Defibrillator (ICD)
For individuals at high risk of recurrent ventricular fibrillation, an implantable cardioverter defibrillator (ICD) may be recommended. This device is implanted under the skin and can automatically detect abnormal heart rhythms and deliver shocks to restore a normal rhythm.
5. Coronary Artery Bypass Surgery or Angioplasty
If VF is caused by coronary artery disease or a heart attack, procedures such as angioplasty or coronary artery bypass surgery may be necessary to restore blood flow to the heart muscle and prevent further arrhythmias.
Preventive Measures for Ventricular Fibrillation
Preventing ventricular fibrillation involves managing the underlying conditions that increase the risk of developing VF, such as coronary artery disease, heart failure, and electrolyte imbalances.
1. Control Risk Factors
Managing risk factors like high blood pressure, high cholesterol, smoking, and diabetes is essential for reducing the risk of developing coronary artery disease and other heart conditions that can lead to VF.
2. Regular Exercise
Regular physical activity helps improve cardiovascular health and reduce the risk of heart disease. However, individuals with existing heart conditions should consult their doctor before engaging in vigorous exercise.
3. Medication Adherence
For individuals with heart conditions or arrhythmias, taking prescribed medications as directed can help prevent complications like VF. Medications may include beta-blockers, ACE inhibitors, and anti-arrhythmic drugs.
4. Routine Heart Check-ups
Regular check-ups with a healthcare provider can help detect early signs of heart disease or arrhythmias, allowing for prompt intervention and treatment.
5. Use of ICDs in High-Risk Individuals
For individuals with a history of heart disease or previous episodes of VF, an ICD may be recommended to prevent sudden cardiac arrest and reduce the risk of recurrence.
Conclusion
Ventricular fibrillation is a serious and potentially fatal condition that requires immediate medical intervention.
Understanding the causes, symptoms, and treatment options for VF is crucial for reducing the risk and improving outcomes for affected individuals. Early diagnosis, prompt defibrillation, and appropriate preventive measures can save lives and help manage this dangerous arrhythmia.
Related topics: