The human cardiovascular system is a complex network of blood vessels that plays a vital role in maintaining overall health.
Understanding the concept of arterial blockage is crucial for recognizing the early signs of cardiovascular disease, which remains a leading cause of morbidity and mortality worldwide. This article aims to explore the concept of arterial blockage, its implications for cardiovascular health, and what constitutes “normal” levels of blockage in the arteries.
The Cardiovascular System: An Overview
Before delving into the specifics of arterial blockage, it is essential to understand the structure and function of the cardiovascular system. The heart, arteries, veins, and capillaries work together to transport oxygen, nutrients, and waste products throughout the body.
Anatomy of the Cardiovascular System
Heart: The heart is a muscular organ that pumps blood throughout the body. It consists of four chambers: the right atrium, right ventricle, left atrium, and left ventricle.
Arteries: These blood vessels carry oxygen-rich blood away from the heart to the body. The aorta is the largest artery, branching into smaller arteries that supply blood to various organs.
Veins: Veins return deoxygenated blood back to the heart. They have thinner walls than arteries and often contain valves to prevent backflow.
Capillaries: These tiny blood vessels connect arteries and veins, facilitating the exchange of oxygen, carbon dioxide, nutrients, and waste products.
The Importance of Healthy Arteries
Healthy arteries are essential for maintaining proper blood flow and oxygen delivery to tissues. When arteries become narrowed or blocked, it can lead to various cardiovascular diseases, including.
Coronary Artery Disease (CAD): A condition where the coronary arteries become narrowed due to plaque buildup, leading to reduced blood flow to the heart muscle.
Peripheral Artery Disease (PAD): Affects blood flow to the limbs, often causing pain and mobility issues.
Stroke: Occurs when blood flow to the brain is interrupted, often due to a blocked artery.
Understanding Arterial Blockage
What Causes Arterial Blockage
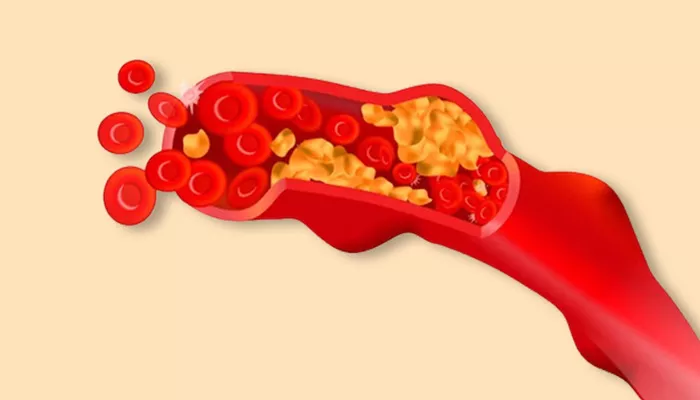
Arterial blockage primarily occurs due to atherosclerosis, a process characterized by the buildup of plaques made up of fat, cholesterol, and other substances on the arterial walls. Several factors contribute to the development of atherosclerosis, including.
High cholesterol levels: Elevated levels of low-density lipoprotein (LDL) cholesterol can lead to plaque formation.
Hypertension: High blood pressure can damage arterial walls, making them more susceptible to plaque buildup.
Smoking: Tobacco use is a significant risk factor for atherosclerosis and cardiovascular disease.
Diabetes: High blood sugar levels can damage blood vessels and accelerate plaque formation.
Obesity: Excess body weight is associated with higher cholesterol levels and increased blood pressure.
Sedentary lifestyle: Lack of physical activity can contribute to obesity and cardiovascular risk.
Genetics: Family history can play a role in an individual’s susceptibility to arterial blockage.
How is Arterial Blockage Measured
Arterial blockage is often assessed using various diagnostic tests, including:
Angiography: A procedure that uses X-rays to visualize blood vessels after injecting a contrast dye. It helps determine the location and severity of blockages.
Ultrasound: This imaging technique uses sound waves to create images of blood vessels and can assess blood flow and plaque buildup.
CT Scans: Computed tomography can provide detailed cross-sectional images of blood vessels and help identify blockages.
Magnetic Resonance Angiography (MRA): This non-invasive imaging technique uses magnetic fields and radio waves to visualize blood vessels.
Interpreting Blockage Levels
Blockage levels are typically expressed as a percentage, indicating the degree to which an artery is narrowed. For example.
0-29% blockage: Generally considered normal; there may be some plaque, but blood flow is not significantly affected.
30-49% blockage: Mild blockage; may not cause noticeable symptoms, but could be a sign of early atherosclerosis.
50-69% blockage: Moderate blockage; may begin to cause symptoms, especially during physical exertion.
70% or more blockage: Severe blockage; often leads to significant symptoms such as chest pain (angina) or shortness of breath and may require medical intervention.
How Much Blockage Is Considered Normal
The “Normal” Range
In general, a blockage of less than 30% in the coronary arteries is considered normal and is often not associated with any symptoms or significant risk for cardiovascular events. However, it is important to note that the presence of plaque, even in small amounts, can indicate an increased risk for future cardiovascular problems.
Risk Factors and Individual Variation
While the above percentages provide a general guideline, individual risk factors play a crucial role in determining what is “normal” for a specific person. For example.
Age: As people age, they are more likely to develop atherosclerosis, and blockages may be more common.
Gender: Men are generally at higher risk for developing coronary artery disease at a younger age compared to women.
Family History: A family history of cardiovascular disease can increase an individual’s risk, making even lower levels of blockage more concerning.
Lifestyle Factors: Diet, exercise, and smoking status can significantly influence an individual’s cardiovascular health and the significance of any arterial blockage.
Symptoms of Arterial Blockage
Recognizing the Signs
Many individuals with arterial blockage may not experience noticeable symptoms, especially in the early stages. However, as blockage progresses, symptoms may develop, including.
Chest Pain (Angina): A feeling of pressure or tightness in the chest, often triggered by physical activity or emotional stress.
Shortness of Breath: Difficulty breathing, especially during exertion.
Fatigue: Unusual tiredness, particularly during physical activities.
Pain in Other Areas: Discomfort may also be felt in the arms, back, neck, jaw, or stomach.
When to Seek Medical Attention
It is essential to seek medical attention if you experience any of the following:
Persistent chest pain or discomfort
Shortness of breath that occurs unexpectedly or with minimal exertion
Pain or discomfort in the arms, back, neck, jaw, or stomach
Symptoms that worsen over time or occur more frequently
Diagnosis and Management of Arterial Blockage
Diagnostic Approaches
If arterial blockage is suspected, healthcare providers may recommend a range of diagnostic tests, including:
Stress Testing: Evaluates how the heart performs under physical stress and can help identify blockages.
Blood Tests: Assess cholesterol levels, blood sugar, and other markers related to cardiovascular health.
Electrocardiogram (ECG): Measures the electrical activity of the heart and can help identify irregularities.
Treatment Options
The management of arterial blockage depends on the severity and symptoms. Treatment options may include,
Lifestyle Modifications
Diet: A heart-healthy diet low in saturated fats, trans fats, and cholesterol can help manage cholesterol levels and improve cardiovascular health.
Exercise: Regular physical activity can improve heart health and help maintain a healthy weight.
Smoking Cessation: Quitting smoking is one of the most effective ways to reduce cardiovascular risk.
Medications
Statins: These medications help lower cholesterol levels and reduce the risk of plaque buildup.
Antiplatelet Agents: Medications like aspirin can help prevent blood clots from forming.
Beta-Blockers: These can help manage blood pressure and reduce the workload on the heart.
Interventional Procedures
Angioplasty and Stenting: A procedure that involves inserting a balloon to open narrowed arteries and placing a stent to keep them open.
Coronary Artery Bypass Grafting (CABG): A surgical procedure that creates a new pathway for blood flow around blocked arteries.
Monitoring and Follow-Up: Regular follow-up appointments and monitoring of cardiovascular health are essential for managing arterial blockage and preventing complications.
Conclusion
Understanding arterial blockage is crucial for maintaining cardiovascular health. While a blockage of less than 30% is generally considered normal, individual risk factors and lifestyle choices play a significant role in determining overall cardiovascular risk. Early detection and management of arterial blockage can significantly reduce the risk of serious cardiovascular events, such as heart attacks and strokes.
By adopting a heart-healthy lifestyle, seeking regular medical check-ups, and being aware of the symptoms associated with arterial blockage, individuals can take proactive steps toward maintaining their cardiovascular health. If you have concerns about your cardiovascular health or experience any symptoms related to arterial blockage, it is essential to consult with a healthcare professional for appropriate evaluation and management.
Related Topics: