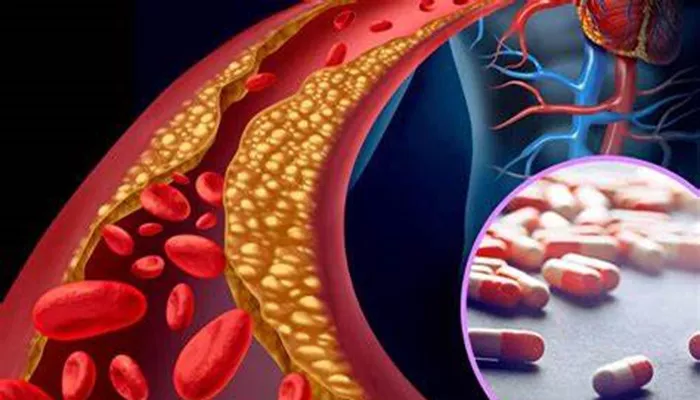
Secondary hyperlipidemia is a type of lipid disorder that arises as a consequence of another underlying health condition, rather than being the primary cause of high cholesterol levels or abnormal lipid profiles. This condition is characterized by abnormal levels of lipids in the blood, including cholesterol and triglycerides. Unlike primary hyperlipidemia, which is often genetically inherited, secondary hyperlipidemia occurs as a result of other diseases, lifestyle factors, or medications that contribute to increased lipid levels.
Hyperlipidemia itself is a well-known risk factor for cardiovascular diseases (CVD) such as heart attacks, strokes, and peripheral artery disease. Therefore, it is crucial to identify and manage secondary hyperlipidemia effectively to prevent long-term complications. This article explores the types, causes, symptoms, diagnosis, treatment methods, and preventive measures for secondary hyperlipidemia, providing a detailed understanding of how it impacts individuals and how healthcare providers can manage it.
Types of Secondary Hyperlipidemia
Secondary hyperlipidemia can be categorized into different types, based on the underlying conditions or factors that contribute to the elevation of lipid levels. The main types include:
Hypercholesterolemia: This is an elevation of low-density lipoprotein (LDL) cholesterol in the blood, commonly known as “bad cholesterol.” It is often seen in individuals with secondary hyperlipidemia due to conditions like hypothyroidism or uncontrolled diabetes.
Hypertriglyceridemia: Elevated levels of triglycerides are a hallmark of hypertriglyceridemia, which is commonly associated with obesity, excessive alcohol consumption, or poorly managed diabetes.
Mixed Hyperlipidemia: This type involves a combination of both high cholesterol and high triglycerides. Conditions such as metabolic syndrome or chronic kidney disease may lead to mixed hyperlipidemia.
Causes of Secondary Hyperlipidemia
Secondary hyperlipidemia occurs due to various underlying conditions, diseases, and lifestyle factors that alter lipid metabolism or increase lipid production in the body. The most common causes include:
1. Diabetes Mellitus
Diabetes, particularly when poorly controlled, can lead to elevated blood sugar levels, which in turn raises triglyceride levels. Additionally, insulin resistance, a hallmark of type 2 diabetes, can decrease the body’s ability to process lipids, contributing to hyperlipidemia.
2. Hypothyroidism
An underactive thyroid gland results in reduced metabolism, which can lead to an increase in cholesterol levels, especially LDL cholesterol. This is because thyroid hormones play a significant role in regulating lipid metabolism.
3. Chronic Kidney Disease
In kidney disease, the body’s ability to remove waste products and excess lipids from the bloodstream is impaired, which can lead to elevated lipid levels. This condition may cause a combination of elevated cholesterol and triglycerides, contributing to mixed hyperlipidemia.
4. Obesity
Obesity, particularly central or abdominal obesity, is a major contributor to secondary hyperlipidemia. Excessive fat in the body alters lipid metabolism and increases triglyceride levels, leading to higher cholesterol and lipid concentrations in the blood.
5. Alcoholism
Chronic alcohol consumption is known to raise triglyceride levels significantly. Alcohol interferes with fat metabolism, leading to elevated lipid levels. Heavy drinking is also associated with liver damage, which can further exacerbate lipid abnormalities.
6. Medications
Certain medications can contribute to secondary hyperlipidemia by increasing lipid production or decreasing lipid breakdown. These include corticosteroids, beta-blockers, diuretics, and some antiretroviral drugs used for HIV treatment.
7. Liver Disease
Liver diseases, such as cirrhosis and non-alcoholic fatty liver disease (NAFLD), can disrupt normal lipid metabolism and cause lipid imbalances. These conditions often lead to increased cholesterol and triglyceride levels.
8. Pregnancy
During pregnancy, hormonal changes can lead to elevated cholesterol and triglyceride levels. This is particularly noticeable in the third trimester and is considered a temporary form of secondary hyperlipidemia that resolves after delivery.
9. Genetic Factors
Although secondary hyperlipidemia is primarily caused by underlying conditions, some individuals may have a genetic predisposition that makes them more susceptible to elevated lipid levels in response to certain diseases or medications.
Symptoms of Secondary Hyperlipidemia
Unlike primary hyperlipidemia, secondary hyperlipidemia often doesn’t present obvious symptoms. Many people may not realize they have this condition until they undergo blood tests to measure their lipid levels. However, there are some signs and symptoms that may suggest the presence of elevated lipids:
Xanthomas: These are fatty deposits that appear as yellowish bumps on the skin, particularly around the eyes, elbows, knees, and hands. They are often associated with high cholesterol levels.
Fatty Liver: In cases of underlying liver disease, individuals may experience symptoms such as fatigue, abdominal pain, and jaundice (yellowing of the skin and eyes).
Chest Pain: High cholesterol and triglycerides contribute to the buildup of plaques in arteries, which can lead to chest pain or angina due to reduced blood flow to the heart.
Numbness or Weakness: High lipid levels can contribute to the development of peripheral artery disease, which may cause numbness, weakness, or pain in the legs due to poor circulation.
Most people with secondary hyperlipidemia, however, will not show noticeable symptoms until significant damage has been done to the cardiovascular system, making regular lipid screening crucial for early detection.
Diagnosis of Secondary Hyperlipidemia
The diagnosis of secondary hyperlipidemia begins with a comprehensive medical history, including an evaluation of any underlying conditions such as diabetes, hypothyroidism, or kidney disease. Blood tests are essential in assessing lipid levels, including:
Lipid Panel: This test measures total cholesterol, LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides. High levels of LDL cholesterol and triglycerides often indicate the presence of secondary hyperlipidemia.
Thyroid Function Tests: For individuals with suspected hypothyroidism, blood tests to measure levels of thyroid-stimulating hormone (TSH) and thyroxine (T4) can help confirm the diagnosis.
Fasting Glucose and HbA1c: Elevated blood glucose levels or poor control of HbA1c (a marker of long-term blood sugar control) can indicate diabetes as an underlying cause of hyperlipidemia.
Kidney Function Tests: Blood tests for creatinine and glomerular filtration rate (GFR) can help assess kidney function, and abnormalities may indicate chronic kidney disease.
Treatment Methods for Secondary Hyperlipidemia
The treatment of secondary hyperlipidemia involves addressing the underlying condition contributing to elevated lipid levels, alongside general lipid-lowering strategies. Treatment options include:
1. Lifestyle Modifications
Dietary Changes: Adopting a heart-healthy diet is crucial in managing secondary hyperlipidemia. This includes reducing saturated fats, eliminating trans fats, increasing fiber intake, and incorporating more fruits, vegetables, and whole grains.
Exercise: Regular physical activity can help lower triglycerides and raise HDL cholesterol. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week.
Weight Loss: For individuals who are obese, losing weight through a combination of diet and exercise can significantly reduce lipid levels and improve overall health.
2. Medications
Statins: These drugs are commonly prescribed to lower LDL cholesterol levels and reduce the risk of cardiovascular disease.
Statins work by inhibiting an enzyme involved in cholesterol production in the liver.
Fibrates: These medications are particularly effective at lowering triglycerides and raising HDL cholesterol.
Ezetimibe: This medication blocks the absorption of cholesterol from the intestine, reducing overall cholesterol levels.
Omega-3 Fatty Acids: High doses of omega-3 fatty acids may be used to lower triglyceride levels in individuals with hypertriglyceridemia.
Thyroid Hormone Replacement: For individuals with hypothyroidism, taking thyroid hormone replacement therapy can normalize cholesterol levels.
3. Management of Underlying Conditions
Diabetes Management: Tight control of blood glucose through lifestyle changes and medications such as insulin or oral hypoglycemics can help lower triglycerides and improve lipid profiles.
Treatment of Kidney Disease: Addressing kidney disease through medications and lifestyle changes can help manage lipid levels and prevent further complications.
4. Monitoring and Follow-Up
Regular follow-up visits with healthcare providers are necessary to monitor lipid levels and the effectiveness of treatment.
Blood tests may be performed every 3-6 months to assess lipid profiles, and adjustments to the treatment plan may be made accordingly.
Preventive Measures for Secondary Hyperlipidemia
Preventing secondary hyperlipidemia involves managing the risk factors that contribute to the development of the underlying conditions. Key preventive measures include:
Regular Health Screenings: Early detection through routine screenings for conditions like diabetes, thyroid disease, and kidney disease can help prevent the onset of secondary hyperlipidemia.
Healthy Lifestyle Choices: Maintaining a healthy weight, eating a balanced diet, exercising regularly, and avoiding excessive alcohol consumption are crucial for preventing both primary and secondary hyperlipidemia.
Managing Chronic Conditions: Effective management of conditions such as diabetes, hypothyroidism, and kidney disease through medications and lifestyle adjustments can significantly reduce the risk of developing secondary hyperlipidemia.
Conclusion
Secondary hyperlipidemia is a significant condition that can lead to serious cardiovascular issues if left untreated. By understanding its causes, symptoms, diagnosis, treatment methods, and preventive strategies, individuals can take proactive steps to manage their health and reduce the risk of developing further complications. Early intervention and appropriate management of underlying conditions are key to controlling lipid levels and improving overall health outcomes. Regular monitoring and a healthy lifestyle are essential in preventing and managing secondary hyperlipidemia, ensuring a better quality of life for those affected.
Related topics: