Mitral regurgitation (MR), also known as mitral insufficiency, is a common heart valve disorder where the mitral valve does not close properly, allowing blood to flow backward into the left atrium instead of moving forward into the left ventricle.
The mitral valve is located between the left atrium and left ventricle, and its primary function is to ensure the unidirectional flow of blood through the heart. When this valve malfunctions, it leads to inefficient blood flow and can place a strain on the heart, potentially resulting in more serious complications if left untreated.
Mitral regurgitation can range from mild to severe and may develop slowly over many years. In some cases, it may not cause symptoms, but in others, it can lead to heart failure and other cardiovascular issues. Early detection and appropriate treatment are essential for managing this condition and preventing long-term complications.
This article provides an in-depth understanding of mitral regurgitation, covering its types, causes, symptoms, diagnostic methods, treatment options, and preventive measures.
Types of Mitral Regurgitation
Mitral regurgitation can be classified based on its underlying cause and the nature of the valve’s dysfunction. The two main types of MR are:
1. Primary (or Organic) Mitral Regurgitation
Primary mitral regurgitation occurs when there is a problem with the mitral valve itself, typically caused by structural abnormalities in the valve or the surrounding structures. The primary causes include:
Mitral Valve Prolapse (MVP): This is the most common cause of primary MR, where the mitral valve flaps (leaflets) bulge (prolapse) backward into the left atrium during contraction of the heart, leading to incomplete closure.
Rheumatic Heart Disease: A complication of a previous streptococcal throat infection, rheumatic fever can cause scarring and deformities in the mitral valve, leading to regurgitation.
Endocarditis: An infection of the heart’s inner lining and valves can damage the mitral valve, leading to MR.
Degenerative Changes: With age, the mitral valve may undergo degenerative changes that cause it to lose its ability to close properly.
Congenital Heart Defects: Some individuals are born with abnormalities in the mitral valve or surrounding structures that lead to MR.
2. Secondary (or Functional) Mitral Regurgitation
Secondary MR occurs due to problems in the heart’s structure that affect the mitral valve’s ability to function properly, even though the valve itself is structurally normal. The main causes of secondary MR include:
Dilated Cardiomyopathy: In this condition, the heart becomes enlarged and weakened, causing the mitral valve to lose its ability to close properly.
Coronary Artery Disease (CAD): Heart attacks or ischemia can lead to damage of the heart muscle, which affects the function of the mitral valve.
Left Ventricular Dysfunction: Conditions that impair the left ventricle’s ability to pump blood, such as heart failure, can lead to a stretching of the heart and subsequent mitral regurgitation.
Causes of Mitral Regurgitation
Mitral regurgitation can occur due to a variety of reasons, both congenital and acquired. The most common causes include:
1. Mitral Valve Prolapse (MVP)
As mentioned, MVP is one of the leading causes of MR, particularly in the primary form. In MVP, one or both of the mitral valve leaflets bulge into the left atrium when the heart contracts, which leads to an incomplete seal and causes blood to leak backward.
2. Rheumatic Fever and Rheumatic Heart Disease
Rheumatic fever, an inflammatory disease caused by a streptococcal throat infection, can lead to rheumatic heart disease, which can damage the mitral valve. Over time, this damage may result in fibrosis, scarring, and stenosis of the mitral valve, contributing to regurgitation.
3. Endocarditis
Infection of the heart’s inner lining, particularly the mitral valve, can result in valve damage. Bacterial endocarditis may cause vegetations (growths of bacteria and clotting material) to form on the valve leaflets, which can lead to regurgitation.
4. Ischemic Heart Disease
Coronary artery disease (CAD) can lead to ischemia or reduced blood flow to the heart muscle. This may result in left ventricular dilation and displacement of the mitral valve, which can prevent the valve from closing properly.
5. Heart Failure
Left ventricular dysfunction in heart failure can cause the heart to dilate, altering the mitral valve’s geometry and causing secondary MR. In this case, the problem is not with the valve itself but with the heart’s inability to function properly.
6. Trauma
Injuries to the chest, such as from a car accident, can damage the mitral valve or the surrounding structures, resulting in regurgitation.
7. Genetic Disorders
Certain genetic conditions, such as Marfan syndrome or Ehlers-Danlos syndrome, can lead to defects in the connective tissues of the heart valves, including the mitral valve, making them more susceptible to prolapse and regurgitation.
Symptoms of Mitral Regurgitation
Mitral regurgitation may be asymptomatic, particularly in the early stages or when the condition is mild. However, as the disease progresses or becomes more severe, individuals may begin to experience symptoms. Common symptoms of mitral regurgitation include:
Fatigue: Individuals with MR may experience general fatigue or a feeling of tiredness due to the heart’s reduced efficiency in pumping blood.
Shortness of Breath: As MR worsens, the heart’s ability to pump blood effectively diminishes, leading to fluid buildup in the lungs and causing shortness of breath, particularly during physical activity or when lying flat.
Palpitations: Patients may feel a fluttering sensation in the chest, often due to irregular heart rhythms (arrhythmias), which can be a complication of MR.
Swelling in the Legs and Abdomen: Severe MR can cause fluid retention, leading to swelling in the lower extremities and abdomen.
Chest Pain: Though rare, chest pain can occur if the left atrium becomes enlarged or if there is an associated ischemic heart disease.
Coughing: In more severe cases, fluid buildup in the lungs may lead to persistent coughing, especially when lying down.
Auscultation Findings
A healthcare provider may hear characteristic heart sounds, such as a “holosystolic murmur,” during auscultation with a stethoscope. This murmur is a hallmark of mitral regurgitation and occurs when blood leaks backward through the mitral valve during the contraction of the heart.
Diagnosis of Mitral Regurgitation
The diagnosis of mitral regurgitation involves several steps, including clinical evaluation, imaging studies, and tests to assess heart function.
The most commonly used diagnostic tools are:
1. Physical Examination
The healthcare provider will listen for a characteristic murmur during a physical examination. The murmur is often heard as a high-pitched, holosystolic sound that is most audible at the apex of the heart.
2. Echocardiography
Echocardiography is the gold standard for diagnosing mitral regurgitation. It uses sound waves to create detailed images of the heart’s structure and function, allowing the provider to assess the mitral valve’s movement, the extent of regurgitation, and any associated heart enlargement.
Transthoracic Echocardiogram (TTE): This is the most commonly performed echocardiogram, where a probe is placed on the chest to obtain images of the heart.
Transesophageal Echocardiogram (TEE): In some cases, a more detailed image of the heart may be obtained using a TEE, which involves a probe inserted into the esophagus to provide clearer images of the mitral valve.
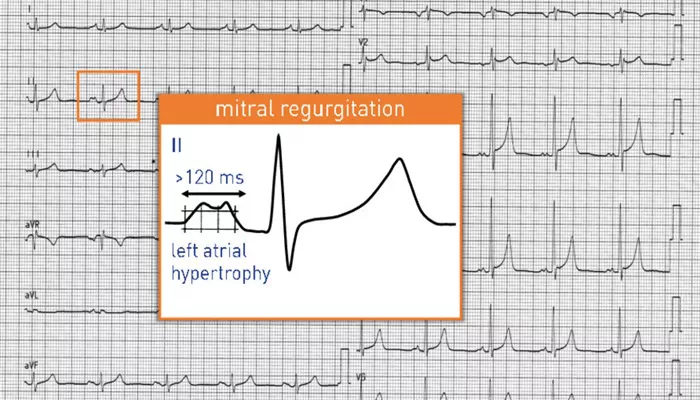
3. Electrocardiogram (ECG)
An ECG may be performed to check for arrhythmias, which can be a complication of MR. It records the electrical activity of the heart.
4. Chest X-ray
A chest X-ray can help determine whether there is any enlargement of the heart or fluid in the lungs, which may be signs of severe MR.
5. Cardiac Catheterization
In some cases, a cardiac catheterization may be performed to assess the severity of MR and the overall condition of the coronary arteries.
Treatment Methods for Mitral Regurgitation
The treatment of mitral regurgitation depends on the severity of the condition, the underlying cause, and the presence of symptoms.
Treatment options include:
1. Medications
Diuretics: These medications help reduce fluid retention, alleviate swelling, and decrease the burden on the heart.
ACE Inhibitors/ARBs: Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are used to lower blood pressure and reduce the workload on the heart.
Beta-Blockers: These drugs can be used to control heart rate and reduce the risk of arrhythmias.
2. Surgical Repair or Replacement
In severe cases, surgical intervention may be necessary to treat MR.
There are two main approaches:
Mitral Valve Repair: If the valve is structurally sound, it may be surgically repaired to restore its proper function.
Mitral Valve Replacement: If repair is not possible, the damaged valve may be replaced with a mechanical or biological valve.
3. Percutaneous Mitral Valve Repair
In some cases, a less invasive procedure called percutaneous mitral valve repair (MitraClip) may be performed. This procedure involves the use of a device inserted through a catheter to clip the mitral valve together, reducing regurgitation.
Preventive Measures for Mitral Regurgitation
While it is not always possible to prevent mitral regurgitation, certain measures can help reduce the risk or slow the progression of the condition:
Managing Risk Factors: Controlling conditions such as high blood pressure, diabetes, and high cholesterol can reduce the strain on the heart and lower the risk of developing MR.
Regular Monitoring: Individuals with mild MR should have regular follow-up appointments to monitor the progression of the condition and detect any worsening symptoms early.
Prompt Treatment of Heart Infections: Preventing and treating infections, such as streptococcal throat infections, can reduce the risk of developing rheumatic heart disease, a major cause of MR.
Lifestyle Modifications: Maintaining a healthy weight, eating a heart-healthy diet, and avoiding smoking can help maintain overall cardiovascular health.
Conclusion
Mitral regurgitation is a common and potentially serious heart valve disorder. While it may be asymptomatic in its early stages, the condition can lead to significant complications if left untreated. Early diagnosis, appropriate treatment, and lifestyle modifications can help manage the condition and prevent further damage to the heart. Regular check-ups and close monitoring are key to ensuring that patients with MR maintain a high quality of life and reduce the risk of severe outcomes.
Related topics: