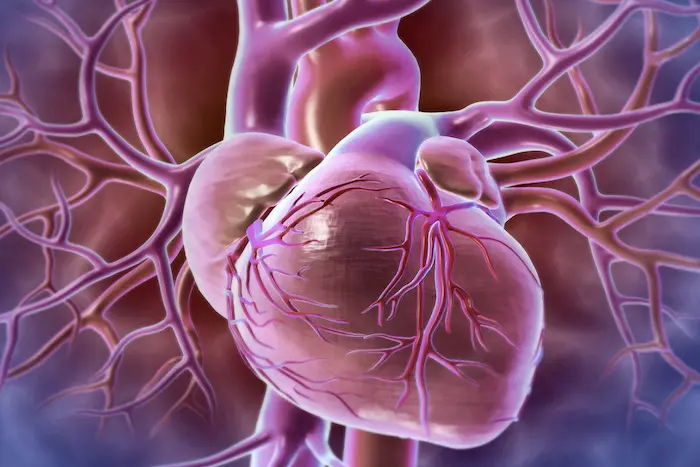
Myocarditis is an inflammatory condition of the heart muscle (myocardium) that can lead to significant cardiovascular complications, including heart failure, arrhythmias, and even sudden cardiac death. One of the most distinctive features of certain types of myocarditis is the presence of giant cells. Giant cells are multinucleated cells that arise from the fusion of macrophages and are often associated with various inflammatory and autoimmune conditions, including giant cell myocarditis (GCM). This article explores the nature of giant cells in myocarditis, their role in the pathophysiology of the disease, the clinical implications of their presence, and the broader context of myocarditis as a whole.
Understanding Myocarditis
Definition and Types
Myocarditis is defined as inflammation of the myocardium, which can result from a variety of causes, including:
Infectious Agents: Viral infections (such as Coxsackievirus, adenovirus, and parvovirus B19) are the most common causes of myocarditis. Bacterial, fungal, and parasitic infections can also lead to myocarditis.
Autoimmune Disorders: Conditions such as systemic lupus erythematosus, rheumatoid arthritis, and sarcoidosis can result in myocarditis due to immune-mediated damage.
Toxins and Drugs: Certain medications, alcohol, and illicit drugs can induce myocarditis.
Idiopathic: In many cases, the exact cause of myocarditis remains unknown.
The types of myocarditis can be classified based on the underlying cause, the histopathological features, and the clinical presentation. Giant cell myocarditis is a specific type characterized by the presence of multinucleated giant cells and is often associated with autoimmune processes.
Pathophysiology of Myocarditis
The pathophysiology of myocarditis involves a complex interplay between infectious agents, the immune response, and myocardial injury. When the heart is exposed to infectious agents or other triggers, the immune system responds by activating inflammatory cells, including macrophages, lymphocytes, and neutrophils. In some cases, this inflammatory response can become dysregulated, leading to extensive myocardial damage.
In giant cell myocarditis, the presence of giant cells is a hallmark feature. These cells are formed by the fusion of activated macrophages in response to persistent inflammation. The presence of giant cells indicates a severe inflammatory process and is often associated with extensive myocardial necrosis and dysfunction.
Giant Cells: Definition and Characteristics
What Are Giant Cells
Giant cells are large, multinucleated cells that arise from the fusion of monocytes or macrophages. They are typically formed in response to chronic inflammation and are often seen in various pathological conditions, including infections, granulomatous diseases, and autoimmune disorders.
Types of Giant Cells
There are several types of giant cells, including:
Langhans Giant Cells: Characterized by a horseshoe arrangement of nuclei, these giant cells are commonly found in granulomatous diseases such as tuberculosis.
Foreign Body Giant Cells: These cells form in response to the presence of foreign materials, such as sutures or implants.
Multinucleated Giant Cells in Myocarditis: In the context of myocarditis, giant cells are typically formed from activated macrophages in response to persistent inflammation and are indicative of severe myocardial damage.
Role of Giant Cells in Myocarditis
In giant cell myocarditis, the presence of giant cells is a key feature that reflects the underlying inflammatory process. The formation of these cells is associated with.
Chronic Inflammation: Giant cells are indicative of a prolonged inflammatory response, suggesting that the immune system is actively trying to eliminate an ongoing insult to the myocardium.
Tissue Damage: The presence of giant cells is often associated with extensive myocardial necrosis and dysfunction, leading to impaired cardiac function.
Immune Activation: Giant cells are a sign of immune activation and may play a role in the pathogenesis of autoimmune myocarditis, where the body’s immune system mistakenly attacks its own heart tissue.
Clinical Presentation of Giant Cell Myocarditis
Symptoms
Patients with giant cell myocarditis may present with a range of symptoms, which can vary in severity:
Chest Pain: Often described as a pressure or tightness in the chest, chest pain can mimic that of a myocardial infarction.
Heart Failure Symptoms: Patients may experience shortness of breath (dyspnea), fatigue, and fluid retention (edema).
Arrhythmias: Irregular heartbeats may occur, leading to palpitations, syncope (fainting), or even sudden cardiac arrest in severe cases.
Generalized Symptoms: Fever, malaise, and other systemic symptoms may be present due to the underlying inflammatory process.
Diagnosis
Diagnosing giant cell myocarditis can be challenging due to its rarity and the overlap of symptoms with other cardiac conditions. The diagnostic approach typically includes.
Clinical History and Physical Examination: A thorough history and physical examination can help identify risk factors and symptoms suggestive of myocarditis.
Electrocardiogram (ECG): An ECG may reveal abnormalities such as ST-segment changes, arrhythmias, or signs of left ventricular hypertrophy.
Echocardiography: This imaging modality can assess cardiac function, wall motion abnormalities, and the presence of pericardial effusion.
Cardiac Magnetic Resonance Imaging (MRI): Cardiac MRI can provide detailed images of the heart and help identify areas of inflammation and scarring.
Endomyocardial Biopsy: The definitive diagnosis of giant cell myocarditis is made through an endomyocardial biopsy, which involves taking a small sample of heart tissue for histopathological examination. The presence of multinucleated giant cells, inflammatory infiltrates, and myocyte necrosis confirms the diagnosis.
Treatment Options for Giant Cell Myocarditis
Medical Management
The management of giant cell myocarditis typically involves a combination of pharmacological therapies aimed at reducing inflammation, managing heart failure symptoms, and preventing arrhythmias.
Immunosuppressive Therapy: Given the autoimmune nature of GCM, immunosuppressive agents such as corticosteroids (prednisone) are commonly used to reduce inflammation. In some cases, additional immunosuppressive agents such as azathioprine or mycophenolate mofetil may be added to the treatment regimen.
Heart Failure Management: Patients with heart failure symptoms may benefit from diuretics, angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, and aldosterone antagonists to improve cardiac function and alleviate symptoms.
Arrhythmia Management: Antiarrhythmic medications may be prescribed to manage arrhythmias, and in severe cases, implantable cardioverter-defibrillators (ICDs) may be necessary to prevent sudden cardiac death.
Advanced Therapies
For patients with severe heart failure or those who do not respond to medical therapy, advanced treatment options may be considered.
Mechanical Circulatory Support: Devices such as ventricular assist devices (VADs) may be used to support cardiac function in patients awaiting heart transplantation.
Heart Transplantation: In cases of refractory heart failure or severe cardiac dysfunction, heart transplantation may be the only viable option for long-term survival.
Prognosis and Long-Term Outcomes
Outcomes
The prognosis for patients with giant cell myocarditis can vary widely depending on the severity of the disease, the timeliness of diagnosis, and the effectiveness of treatment. Historically, GCM has been associated with a poor prognosis, with reported mortality rates ranging from 30% to 50% within the first year of diagnosis.
Factors Influencing Prognosis
Several factors can influence the prognosis of giant cell myocarditis:
Early Diagnosis and Treatment: Early recognition and prompt initiation of immunosuppressive therapy can significantly improve outcomes.
Response to Treatment: Patients who respond well to immunosuppressive therapy tend to have better long-term outcomes compared to those who do not.
Presence of Comorbidities: The presence of other medical conditions, such as diabetes or chronic kidney disease, can negatively impact prognosis.
Long-Term Follow-Up
Long-term follow-up is essential for patients with giant cell myocarditis, as they may be at risk for recurrent episodes of myocarditis or the development of heart failure. Regular monitoring of cardiac function, symptom assessment, and adjustments to treatment plans are crucial for optimizing outcomes.
Conclusion
Giant cells play a critical role in the pathophysiology of giant cell myocarditis, serving as markers of severe inflammation and myocardial damage. Understanding the nature and significance of giant cells in myocarditis is essential for healthcare providers, as it informs diagnosis, treatment, and prognostic considerations.
Giant cell myocarditis is a rare but serious condition that poses significant challenges for diagnosis and management. The presence of giant cells reflects an active and aggressive inflammatory process that can lead to severe cardiac dysfunction and poor outcomes. Early recognition, prompt treatment, and ongoing monitoring are essential for improving the prognosis of affected individuals.
As research continues to evolve, it is essential to maintain a focus on understanding the underlying mechanisms of giant cell myocarditis, identifying potential risk factors, and exploring novel therapeutic approaches. Increased awareness and education within the medical community will ultimately contribute to improved recognition and management of this complex and challenging condition, enhancing the quality of care for affected individuals.
Related Topics: