Pulmonary hypertension (PH) is a complex and serious condition characterized by elevated blood pressure in the pulmonary arteries, which supply blood from the heart to the lungs. This increase in pressure can lead to significant complications, including heart failure, reduced exercise capacity, and decreased quality of life. Among the various types of pulmonary hypertension, one form stands out as the most common: pulmonary arterial hypertension (PAH). This article explores the nature of pulmonary hypertension, with a focus on pulmonary arterial hypertension, including its causes, symptoms, diagnosis, treatment, and implications for patient health.
Understanding Pulmonary Hypertension
Definition
Pulmonary hypertension is defined as a mean pulmonary arterial pressure (mPAP) greater than 25 mmHg at rest, as measured by right heart catheterization. Normal pulmonary arterial pressure is typically around 8 to 20 mmHg. The condition can be classified into five groups based on the underlying causes, as outlined by the World Health Organization (WHO).
Group 1: Pulmonary Arterial Hypertension (PAH)
Group 2: Pulmonary Hypertension due to Left Heart Disease
Group 3: Pulmonary Hypertension due to Lung Diseases and/or Hypoxia
Group 4: Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
Group 5: Pulmonary Hypertension with Unclear Multifactorial Mechanisms
Among these, Group 1, or pulmonary arterial hypertension, is the most common form of pulmonary hypertension.
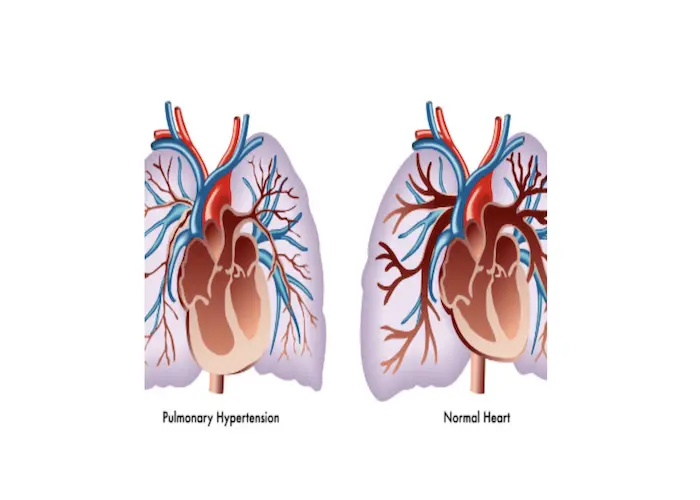
Pathophysiology
In pulmonary arterial hypertension, the small arteries in the lungs become narrowed, blocked, or destroyed, leading to increased resistance to blood flow. This increased resistance causes the right ventricle to work harder to pump blood through the lungs, ultimately leading to right ventricular hypertrophy and, in severe cases, right heart failure.
Causes of Pulmonary Arterial Hypertension
Idiopathic Pulmonary Arterial Hypertension
Idiopathic pulmonary arterial hypertension (IPAH) has no identifiable cause and is the most common subtype of PAH. It is often diagnosed in young to middle-aged adults, particularly women.
Heritable Pulmonary Arterial Hypertension
Heritable PAH is associated with genetic mutations, particularly in the BMPR2 gene. Individuals with a family history of PAH are at increased risk.
Associated Conditions
Several conditions can lead to the development of PAH, including:
Connective Tissue Diseases: Conditions such as systemic sclerosis (scleroderma), lupus, and rheumatoid arthritis can increase the risk of PAH.
Congenital Heart Disease: Certain congenital heart defects, such as atrial septal defects, can lead to increased blood flow to the pulmonary arteries and subsequent hypertension.
Portal Hypertension: Liver diseases, including cirrhosis, can lead to the development of PAH.
HIV Infection: Human immunodeficiency virus (HIV) infection has been associated with an increased risk of developing PAH.
Drugs and Toxins: Certain medications, including some appetite suppressants and illegal drugs like cocaine, have been linked to PAH.
Symptoms of Pulmonary Arterial Hypertension
The symptoms of PAH can be subtle and may initially be mistaken for other conditions. Common symptoms include.
Shortness of Breath (Dyspnea): Often occurring during exertion and, as the disease progresses, at rest.
Fatigue: A general feeling of tiredness and lack of energy.
Chest Pain: Discomfort or pain in the chest, which may mimic angina.
Palpitations: Awareness of an irregular or rapid heartbeat.
Swelling (Edema): Particularly in the ankles and legs due to fluid retention.
Cyanosis: A bluish tint to the lips and skin, indicating inadequate oxygenation.
Diagnosis of Pulmonary Arterial Hypertension
Clinical Evaluation
Diagnosing PAH involves a comprehensive clinical evaluation, including:
Medical History: Gathering information on symptoms, family history, and potential risk factors.
Physical Examination: Checking for signs of right heart failure, such as elevated jugular venous pressure and peripheral edema.
Diagnostic Tests
Echocardiography: This non-invasive imaging test can estimate pulmonary artery pressure and assess right ventricular function. While it is not definitive, it is often the first test performed.
Right Heart Catheterization: This is the gold standard for diagnosing PAH. It involves inserting a catheter into the right side of the heart and measuring pressures in the pulmonary arteries directly.
Pulmonary Function Tests: These tests evaluate lung function and can help rule out other causes of dyspnea.
Chest Imaging: Chest X-rays and CT scans can help identify underlying lung diseases or structural abnormalities.
Blood Tests: Blood tests can help assess for underlying conditions, such as connective tissue diseases or liver disease.
Treatment of Pulmonary Arterial Hypertension
Pharmacological Treatments
The management of pulmonary arterial hypertension involves various pharmacological treatments aimed at improving symptoms and slowing disease progression. Key classes of medications include.
Endothelin Receptor Antagonists (ERAs): These medications, such as bosentan and ambrisentan, block the effects of endothelin, a potent vasoconstrictor, helping to dilate pulmonary and systemic arterial vascular beds.
Phosphodiesterase-5 Inhibitors (PDE-5 Inhibitors): Medications like sildenafil and tadalafil enhance the effects of nitric oxide, leading to vasodilation and improved blood flow.
Prostacyclin Analogues: These medications, such as epoprostenol and treprostinil, mimic the effects of prostacyclin, a natural vasodilator. They can be administered via infusion, inhalation, or oral routes.
Soluble Guanylate Cyclase Stimulators: Riociguat is a medication that stimulates the soluble guanylate cyclase pathway, leading to increased levels of cyclic GMP and vasodilation.
Anticoagulants: Patients with PAH may be at increased risk for blood clots, and anticoagulants may be prescribed to reduce this risk.
Non-Pharmacological Treatments
Oxygen Therapy: Supplemental oxygen may be needed for patients with low oxygen saturation levels.
Pulmonary Rehabilitation: A structured program that includes exercise training, education, and support to improve physical function and quality of life.
Surgical Interventions: In select cases, surgical options such as atrial septostomy or lung transplantation may be considered for patients with severe PAH that is refractory to medical therapy.
Living with Pulmonary Arterial Hypertension
Lifestyle Modifications
Dietary Changes: A heart-healthy diet low in sodium can help manage fluid retention and blood pressure.
Regular Exercise: Engaging in regular, supervised exercise can improve cardiovascular fitness and overall well-being.
Avoiding High Altitudes: High altitudes can exacerbate symptoms of PAH due to lower oxygen levels.
Stress Management: Techniques such as mindfulness, meditation, and counseling can help manage stress, which may worsen symptoms.
Monitoring and Follow-Up
Regular follow-up appointments are essential for monitoring disease progression, adjusting treatment plans, and managing symptoms. Patients should be educated about recognizing signs of worsening PAH and when to seek medical attention.
Prognosis and Outcomes
The prognosis for patients with pulmonary arterial hypertension has improved significantly over the past few decades due to advances in diagnosis and treatment. However, PAH remains a serious condition with a variable prognosis depending on several factors, including.
Underlying Cause: Idiopathic PAH may have a different prognosis than PAH associated with connective tissue diseases.
Severity of Symptoms: Patients with more severe symptoms at diagnosis generally have a poorer prognosis.
Response to Treatment: Patients who respond well to therapy tend to have better outcomes.
Survival Rates
Historically, the median survival for untreated PAH was less than three years. However, with the advent of effective therapies, the median survival has improved significantly, with many patients living for years with appropriate management.
Conclusion
Pulmonary arterial hypertension (PAH) is the most common form of pulmonary hypertension and a serious condition that can significantly impact patients’ lives. Understanding the causes, symptoms, diagnosis, and treatment options for PAH is crucial for both patients and healthcare providers.
With advancements in medical therapy and a better understanding of the disease, the prognosis for patients with PAH has improved considerably. Early diagnosis and appropriate management are key to optimizing outcomes and enhancing the quality of life for individuals living with this challenging condition.
As research continues to evolve, it is essential to raise awareness about pulmonary arterial hypertension, promote early detection, and advocate for ongoing education and support for patients and their families. By doing so, we can work towards better health outcomes and improved quality of life for those affected by this complex disease.
Related Topics: