Giant cell myocarditis (GCM) is a rare and severe form of myocarditis characterized by the presence of multinucleated giant cells in the myocardium. This condition can lead to significant cardiac dysfunction and has a poor prognosis if not diagnosed and treated promptly. Diagnosing giant cell myocarditis is challenging due to its nonspecific symptoms and the need for specialized diagnostic techniques. This article provides a comprehensive overview of the diagnostic process for giant cell myocarditis, including clinical evaluation, imaging studies, laboratory tests, and histopathological examination.
Understanding Giant Cell Myocarditis
Definition and Background
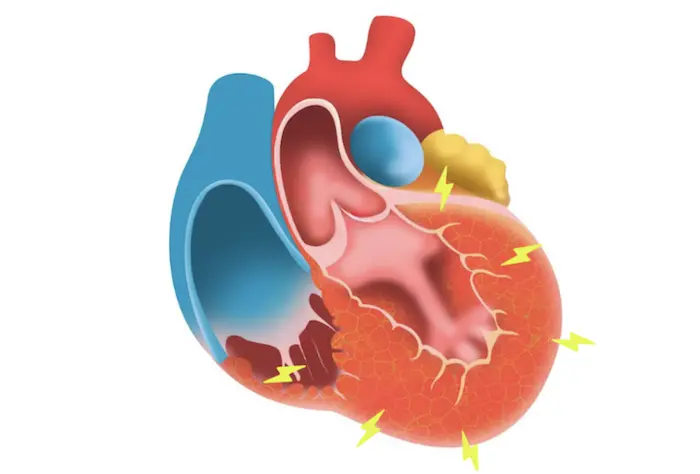
Giant cell myocarditis is an inflammatory disease of the heart muscle, often associated with autoimmune processes. The presence of giant cells—multinucleated cells formed by the fusion of macrophages—distinguishes GCM from other forms of myocarditis. This condition can lead to rapid progression of heart failure, arrhythmias, and sudden cardiac death, making early diagnosis crucial.
Epidemiology
Giant cell myocarditis is a rare condition, with an estimated incidence of 1-2 cases per million people per year. It predominantly affects young to middle-aged adults, with no significant gender predisposition. The exact etiology remains unclear, but it is often associated with other autoimmune diseases, viral infections, and certain genetic predispositions.
Clinical Presentation of Giant Cell Myocarditis
Symptoms
The symptoms of giant cell myocarditis can vary widely but commonly include:
Chest Pain: Patients may experience chest pain that mimics angina or myocardial infarction.
Heart Failure Symptoms: Symptoms such as dyspnea (shortness of breath), fatigue, and peripheral edema may occur due to impaired cardiac function.
Arrhythmias: Patients may present with palpitations, syncope (fainting), or even sudden cardiac arrest due to conduction disturbances.
Systemic Symptoms: Fever, malaise, and other systemic symptoms may be present, reflecting the underlying inflammatory process.
Disease Progression
Giant cell myocarditis can progress rapidly, often leading to severe heart failure or sudden cardiac death within weeks to months of symptom onset. Early recognition and treatment are critical to improving outcomes.
Diagnostic Approach to Giant Cell Myocarditis
Diagnosing giant cell myocarditis involves a multi-step approach that includes clinical evaluation, laboratory tests, imaging studies, and histopathological examination. Each component plays a crucial role in establishing the diagnosis and ruling out other potential causes of myocarditis.
Clinical Evaluation
History Taking
A thorough medical history is essential in the diagnostic process. Key components of the history include.
Symptom Onset and Duration: Understanding when symptoms began and their progression can help assess the severity of the disease.
Previous Medical History: A history of autoimmune diseases, viral infections, or recent vaccinations can provide important clues.
Family History: A family history of autoimmune diseases or sudden cardiac events may suggest a genetic predisposition.
Social History: Information about lifestyle factors, such as smoking, alcohol use, and physical activity, can also be relevant.
Physical Examination
A comprehensive physical examination can help identify signs of heart failure and systemic involvement. Key findings may include.
Vital Signs: Tachycardia, hypotension, or fever may be present.
Cardiac Exam: A murmur or abnormal heart sounds may indicate structural heart disease.
Pulmonary Exam: Rales or decreased breath sounds may suggest pulmonary congestion.
Peripheral Edema: Swelling in the extremities can indicate fluid retention due to heart failure.
Electrocardiogram (ECG)
An electrocardiogram (ECG) is a vital tool in the initial evaluation of patients suspected of having myocarditis. It can reveal various abnormalities, including.
ST-Segment Changes: Elevation or depression may indicate myocardial injury.
Arrhythmias: Atrial fibrillation, ventricular tachycardia, or other arrhythmias may be present, reflecting underlying myocardial damage.
Conduction Abnormalities: Bundle branch block or atrioventricular block can occur due to inflammation and scarring of the conduction system.
Laboratory Tests
Various laboratory tests may be performed to support the diagnosis of giant cell myocarditis and rule out other conditions:
Cardiac Biomarkers
Troponin Levels: Elevated troponin levels indicate myocardial injury and are often present in patients with myocarditis.
B-Type Natriuretic Peptide (BNP): Elevated BNP levels can indicate heart failure and provide additional information about cardiac function.
Inflammatory Markers
C-Reactive Protein (CRP): Elevated CRP levels indicate systemic inflammation and may be used to assess disease activity.
Erythrocyte Sedimentation Rate (ESR): Increased ESR can also indicate inflammation but is nonspecific.
Autoimmune Panel
Antinuclear Antibodies (ANA): A positive ANA test may indicate an underlying autoimmune process.
Other Autoantibodies: Testing for specific autoantibodies, such as anti-Ro or anti-La, may be considered depending on the clinical context.
Imaging Studies
Imaging studies play a crucial role in assessing cardiac function and identifying structural abnormalities. The following modalities are commonly used.
Echocardiography
Role: Echocardiography is a non-invasive imaging technique that can assess cardiac structure and function.
Findings: It may reveal left ventricular dysfunction, wall motion abnormalities, and the presence of pericardial effusion.
Limitations: While echocardiography can provide valuable information, it may not be specific for diagnosing giant cell myocarditis.
Cardiac Magnetic Resonance Imaging (MRI)
Role: Cardiac MRI is a powerful imaging modality that can provide detailed information about myocardial inflammation and scarring.
Findings: Key features of giant cell myocarditis on cardiac MRI include:
Myocardial Edema: Increased signal intensity on T2-weighted images indicates edema.
Late Gadolinium Enhancement (LGE): This finding indicates myocardial fibrosis and can help differentiate between various types of myocarditis.
Advantages: Cardiac MRI is particularly useful for assessing the extent of myocardial involvement and can guide treatment decisions.
Endomyocardial Biopsy
The definitive diagnosis of giant cell myocarditis is made through an endomyocardial biopsy, which involves obtaining a small sample of myocardial tissue for histopathological examination. This procedure is often performed in cases where the diagnosis is uncertain or when the patient presents with severe symptoms.
Procedure
Indications: An endomyocardial biopsy is indicated in patients with suspected myocarditis who have severe heart failure, arrhythmias, or when the diagnosis is unclear after non-invasive testing.
Technique: The biopsy is typically performed via a catheter inserted through the femoral vein and advanced to the right side of the heart. Multiple samples may be taken to increase diagnostic yield.
Histopathological Examination
Findings: Histopathological examination of the biopsy samples may reveal:
Multinucleated Giant Cells: The presence of these cells is characteristic of giant cell myocarditis.
Lymphocytic Infiltrate: Inflammatory infiltrates consisting primarily of lymphocytes may also be observed.
Myocyte Necrosis: Evidence of myocardial cell death can indicate active inflammation.
Differential Diagnosis: The biopsy can help differentiate giant cell myocarditis from other forms of myocarditis, such as viral myocarditis or sarcoidosis, based on the histological findings.
Differential Diagnosis
When diagnosing giant cell myocarditis, it is essential to differentiate it from other conditions that can present with similar symptoms. Key differential diagnoses include.
Viral Myocarditis: Often characterized by a lymphocytic infiltrate without giant cells.
Autoimmune Myocarditis: Conditions such as systemic lupus erythematosus or rheumatoid arthritis may also involve the myocardium but have distinct histopathological features.
Sarcoidosis: This systemic granulomatous disease can affect the heart but typically presents with non-caseating granulomas rather than giant cells.
Ischemic Heart Disease: Patients with coronary artery disease may present with similar symptoms, but the underlying etiology differs.
Conclusion
Diagnosing giant cell myocarditis is a complex process that requires a comprehensive approach, combining clinical evaluation, imaging studies, laboratory tests, and histopathological examination. Given the aggressive nature of this condition and its potential for rapid progression, early recognition and diagnosis are crucial for improving patient outcomes.
Healthcare providers must maintain a high index of suspicion for giant cell myocarditis, particularly in young to middle-aged patients presenting with unexplained heart failure or arrhythmias. A multidisciplinary approach involving cardiologists, pathologists, and radiologists is essential to ensure accurate diagnosis and timely management.
As research continues to evolve, there is hope for improved diagnostic techniques and therapeutic strategies for giant cell myocarditis. Ongoing advancements in imaging modalities, biomarker discovery, and understanding of the underlying immunopathology will further enhance our ability to diagnose and treat this challenging condition. Ultimately, early diagnosis and intervention can significantly improve the quality of life and survival for patients facing giant cell myocarditis.
Related Topics: