Congestive Heart Failure (CHF) is a chronic, progressive condition that affects the heart’s ability to pump blood efficiently.
It is a leading cause of morbidity and mortality worldwide. One of the most critical aspects of managing CHF is understanding the concept of exacerbation, which refers to a sudden worsening of symptoms that can lead to hospitalization and increased healthcare costs. This article will explore what CHF exacerbation means, its causes, symptoms, diagnosis, treatment strategies, and the importance of effective management to prevent exacerbations.
Understanding Congestive Heart Failure (CHF)
Definition of CHF
Congestive Heart Failure is defined as a clinical syndrome characterized by the heart’s inability to pump sufficient blood to meet the body’s metabolic needs. This condition can result from various structural and functional abnormalities of the heart, leading to a range of symptoms that affect the patient’s quality of life.
Types of CHF
CHF can be classified into two main types based on the heart’s function:
Systolic Heart Failure: This occurs when the heart muscle is weakened and cannot contract effectively, resulting in a reduced ejection fraction (EF) of less than 40%.
Diastolic Heart Failure: In this type, the heart muscle becomes stiff and cannot relax properly, leading to inadequate filling of the heart chambers. Patients may have a normal EF but still experience symptoms of heart failure.
Stages of CHF
CHF is also classified into stages based on the severity of the condition, ranging from Stage A (at risk for heart failure) to Stage D (advanced heart failure). Understanding these stages is crucial for managing exacerbations effectively.
What Is CHF Exacerbation
Definition of Exacerbation
CHF exacerbation refers to a sudden worsening of heart failure symptoms that can lead to increased fluid retention, decreased exercise tolerance, and the need for medical intervention. This exacerbation can manifest as an acute episode requiring hospitalization or can be managed on an outpatient basis, depending on the severity of the symptoms.
Causes of CHF Exacerbation
Several factors can trigger an exacerbation of CHF, including:
Non-Adherence to Medication: Failure to take prescribed medications as directed can lead to fluid overload and worsening symptoms.
Dietary Changes: Increased sodium intake from diet can cause fluid retention, exacerbating heart failure symptoms.
Infections: Respiratory infections, urinary tract infections, and other illnesses can stress the heart and lead to exacerbation.
Arrhythmias: Irregular heartbeats can compromise cardiac output and lead to worsening heart failure symptoms.
Uncontrolled Hypertension: High blood pressure can increase the workload on the heart, contributing to exacerbation.
Myocardial Ischemia: Reduced blood flow to the heart muscle can lead to worsening heart function and exacerbation.
Physical Inactivity: Lack of physical activity can lead to deconditioning, making it harder for the heart to cope with daily activities.
Emotional Stress: Stress and anxiety can trigger physiological responses that worsen heart failure symptoms.
Weather Changes: Extreme temperatures, particularly heat, can exacerbate heart failure symptoms due to increased fluid retention and strain on the heart.
Symptoms of CHF Exacerbation
Recognizing the symptoms of CHF exacerbation is crucial for timely intervention. Common symptoms include.
Increased Shortness of Breath: Patients may experience worsening dyspnea, especially during physical activity or while lying flat (orthopnea).
Increased Fatigue: A sudden increase in fatigue or weakness can indicate worsening heart failure.
Swelling: Edema in the legs, ankles, or abdomen may become more pronounced due to fluid retention.
Persistent Cough: A cough that produces pink, frothy sputum can indicate pulmonary congestion.
Rapid Weight Gain: A sudden increase in weight (more than 2-3 pounds in a day or 5 pounds in a week) may indicate fluid retention.
Increased Heart Rate: Patients may notice palpitations or a rapid heartbeat.
Dizziness or Confusion: Reduced blood flow to the brain can lead to cognitive changes.
Decreased Urination: A reduction in urine output may indicate worsening fluid retention.
Diagnosing CHF Exacerbation
Medical History and Physical Examination
A thorough medical history and physical examination are essential for diagnosing CHF exacerbation. Healthcare providers will assess the patient’s symptoms, medication adherence, and any recent changes in health or lifestyle.
Diagnostic Tests
Several diagnostic tests may be performed to confirm CHF exacerbation and assess its severity:
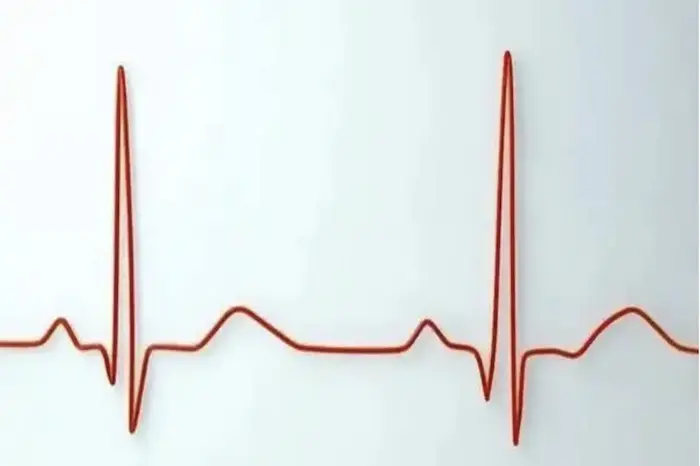
Electrocardiogram (ECG): This test measures the heart’s electrical activity and can identify arrhythmias or previous heart damage.
Echocardiogram: An ultrasound of the heart provides information about its structure and function, including ejection fraction and chamber sizes.
Chest X-ray: A chest X-ray can reveal signs of fluid in the lungs or heart enlargement.
Blood Tests: Measurement of biomarkers such as B-type natriuretic peptide (BNP) or N-terminal pro B-type natriuretic peptide (NT-proBNP) can help confirm heart failure exacerbation.
Urinalysis: A urine test may be conducted to check for signs of kidney function and fluid retention.
Treatment of CHF Exacerbation
Immediate Management
The immediate management of CHF exacerbation focuses on relieving symptoms and stabilizing the patient. Key interventions include.
Diuretics: Administering diuretics helps to reduce fluid overload and alleviate symptoms of congestion. Loop diuretics, such as furosemide, are commonly used.
Oxygen Therapy: Supplemental oxygen may be provided to improve oxygen saturation, especially in patients experiencing significant shortness of breath.
Blood Pressure Management: Medications may be adjusted to manage blood pressure and reduce the heart’s workload.
Intravenous Medications: In severe cases, intravenous medications may be necessary to quickly manage symptoms and stabilize heart function.
Long-Term Management
After stabilization, long-term management strategies are essential to prevent future exacerbations:
Medication Optimization: Reviewing and adjusting heart failure medications, including ACE inhibitors, beta-blockers, and aldosterone antagonists, can improve outcomes.
Patient Education: Educating patients about recognizing early signs of exacerbation, medication adherence, and lifestyle modifications is crucial.
Dietary Modifications: Encouraging a low-sodium diet can help prevent fluid retention and exacerbation.
Regular Monitoring: Routine follow-up appointments and monitoring of weight, blood pressure, and symptoms can help detect early signs of exacerbation.
Cardiac Rehabilitation: Structured exercise programs can improve cardiovascular fitness and overall well-being.
Psychosocial Support: Addressing emotional and psychological factors through counseling or support groups can help patients cope with their condition.
Preventing CHF Exacerbation
Preventing exacerbations of CHF requires a multifaceted approach that includes:
Adherence to Treatment: Patients must take medications as prescribed and attend regular follow-up appointments.
Monitoring Symptoms: Keeping track of weight, symptoms, and any changes in health can help detect early signs of exacerbation.
Healthy Lifestyle Choices: Adopting a heart-healthy diet, engaging in regular physical activity, and avoiding smoking and excessive alcohol consumption can help manage CHF effectively.
Managing Comorbid Conditions: Proper management of conditions such as hypertension, diabetes, and obesity is essential for preventing exacerbations.
Education and Awareness: Patients and caregivers should be educated about CHF, its symptoms, and the importance of early intervention.
Conclusion
CHF exacerbation is a significant concern for patients and healthcare providers, as it can lead to increased morbidity, hospitalizations, and healthcare costs. Understanding what CHF exacerbation means, its causes, symptoms, diagnostic criteria, and treatment strategies is essential for effective management.
By recognizing the early signs of exacerbation and implementing appropriate interventions, patients can improve their quality of life and reduce the risk of hospitalization. Effective management requires a comprehensive approach that includes medication optimization, lifestyle modifications, patient education, and regular monitoring.
As the healthcare landscape continues to evolve, ongoing research and advancements in the understanding of CHF will contribute to better management strategies and improved outcomes for patients. Empowering patients with knowledge and resources is key to preventing exacerbations and enhancing their overall health and well-being.
Related Topics: