Mitral regurgitation (MR) is a heart condition that affects the mitral valve, one of the four main valves in the heart. This valve plays a crucial role in ensuring that blood flows in the correct direction within the heart. When the mitral valve doesn’t close properly, blood flows backward into the left atrium instead of flowing forward into the left ventricle, a condition known as mitral regurgitation. This backward flow of blood can strain the heart and lead to various complications, making it essential to understand the causes, symptoms, treatment, and preventive measures related to this condition.
In this article, we will explore the fundamentals of mitral regurgitation, including its causes, levels of severity, symptoms, diagnostic methods, treatment options, and preventive strategies.
Understanding The Mitral Valve
Before delving into the specifics of mitral regurgitation, it is essential to understand the function of the mitral valve. The heart consists of four chambers: two atria (upper chambers) and two ventricles (lower chambers). The mitral valve is located between the left atrium and the left ventricle. Its function is to allow blood to flow from the left atrium into the left ventricle while preventing the backward flow of blood when the left ventricle contracts to pump blood into the aorta.
The mitral valve is composed of two leaflets that open and close with each heartbeat. When these leaflets fail to close properly, they allow blood to leak backward into the left atrium. This leakage is known as mitral regurgitation and can cause a variety of issues for the heart.
Causes of Mitral Regurgitation
Mitral regurgitation can occur due to various underlying conditions that affect the structure or function of the mitral valve.
Some of the most common causes include:
1. Mitral Valve Prolapse (MVP)
Mitral valve prolapse is one of the most common causes of mitral regurgitation. It occurs when one or both of the valve leaflets bulge into the left atrium during the contraction of the left ventricle. This bulging causes the valve to close improperly, leading to the backward flow of blood. Mitral valve prolapse can be present from birth or develop as a result of aging, and it may be exacerbated by conditions like connective tissue disorders.
2. Rheumatic Heart Disease
Rheumatic fever, a complication of untreated strep throat, can lead to rheumatic heart disease. This condition damages the heart valves, including the mitral valve, causing it to become scarred and misshapen. The damaged valve may not close properly, leading to mitral regurgitation.
3. Heart Attack (Myocardial Infarction)
A heart attack can damage the heart muscle and the structures associated with the mitral valve. If the heart attack affects the left ventricle, the resulting damage can alter the shape of the ventricle and affect the way the mitral valve functions.
This can lead to mitral regurgitation.
4. Endocarditis
Endocarditis is an infection of the inner lining of the heart, usually caused by bacteria. If the infection affects the mitral valve, it can lead to damage and dysfunction, resulting in mitral regurgitation.
5. Congenital Heart Defects
Some individuals are born with structural abnormalities of the heart, including issues with the mitral valve. These congenital defects can cause the valve to function improperly, leading to mitral regurgitation.
6. Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle, which can affect the structure and function of the heart. In particular, dilated cardiomyopathy (where the heart becomes enlarged and weakened) can lead to mitral regurgitation by stretching and deforming the mitral valve.
7. Aging
As individuals age, the tissues of the mitral valve can become weakened, and the valve may lose some of its flexibility. This natural wear and tear can cause the valve to function improperly, leading to mitral regurgitation.
Levels of Mitral Regurgitation
Mitral regurgitation is classified into different levels based on its severity. The classification helps guide treatment and management decisions. The levels of mitral regurgitation are:
1. Mild Mitral Regurgitation
In mild mitral regurgitation, the backward flow of blood is minimal, and the heart can usually compensate for the condition.
Many individuals with mild mitral regurgitation may not experience symptoms and can live a normal life. However, it is still important to monitor the condition regularly to prevent progression.
2. Moderate Mitral Regurgitation
Moderate mitral regurgitation means that there is a more significant amount of blood leaking back into the left atrium.
While the heart may still be able to compensate, some individuals may begin to experience symptoms such as shortness of breath or fatigue. Regular monitoring and medical intervention are typically necessary.
3. Severe Mitral Regurgitation
In severe mitral regurgitation, a large amount of blood leaks backward into the left atrium, causing the heart to work much harder to pump blood effectively. This can lead to symptoms such as chest pain, palpitations, shortness of breath, and swelling in the legs or abdomen. Severe mitral regurgitation can lead to heart failure and may require surgical intervention.
Symptoms of Mitral Regurgitation
The symptoms of mitral regurgitation can vary depending on the severity of the condition. In the early stages, many individuals with mild or moderate mitral regurgitation may not experience noticeable symptoms. However, as the condition progresses, symptoms may become more apparent.
Common symptoms include:
- Shortness of breath, especially during physical activity or when lying down
- Fatigue and a general feeling of weakness
- Palpitations (a feeling of a rapid or irregular heartbeat)
- Chest pain or discomfort
- Swelling in the legs, ankles, or abdomen (due to fluid retention)
- Dizziness or fainting
Severe mitral regurgitation can lead to heart failure if left untreated, making early detection and management crucial.
Diagnosis of Mitral Regurgitation
The diagnosis of mitral regurgitation typically involves a combination of a physical examination, medical history review, and diagnostic tests.
Common diagnostic procedures include:
1. Physical Examination
During a physical exam, a healthcare provider will listen for abnormal heart sounds, such as a murmur, which is common in individuals with mitral regurgitation. A heart murmur occurs when blood flows through the mitral valve in an abnormal manner.
2. Echocardiogram
An echocardiogram is a key diagnostic tool for diagnosing mitral regurgitation. This non-invasive ultrasound test uses sound waves to create images of the heart’s structures and assess how well the mitral valve is functioning. It can determine the degree of regurgitation and any related damage to the heart.
3. Electrocardiogram (ECG or EKG)
An electrocardiogram records the electrical activity of the heart. It can help identify any abnormal heart rhythms or signs of heart enlargement that may occur as a result of mitral regurgitation.
4. Chest X-ray
A chest X-ray can reveal changes in the size and shape of the heart, which may indicate that the left atrium or left ventricle has been affected by mitral regurgitation.
5. Cardiac MRI
In some cases, a cardiac MRI may be used to provide more detailed images of the heart’s structure and function. This may be necessary for assessing the severity of mitral regurgitation and planning treatment.
Treatment of Mitral Regurgitation
Treatment for mitral regurgitation depends on the severity of the condition and the symptoms the patient is experiencing.
The goal of treatment is to manage symptoms, prevent complications, and improve heart function. Treatment options include:
1. Medications
For individuals with mild to moderate mitral regurgitation, medications may be prescribed to help manage symptoms and reduce the workload on the heart. These medications may include:
- Beta-blockers to control heart rate and reduce strain on the heart
- Diuretics to reduce fluid buildup in the body
- ACE inhibitors or ARBs to relax blood vessels and lower blood pressure
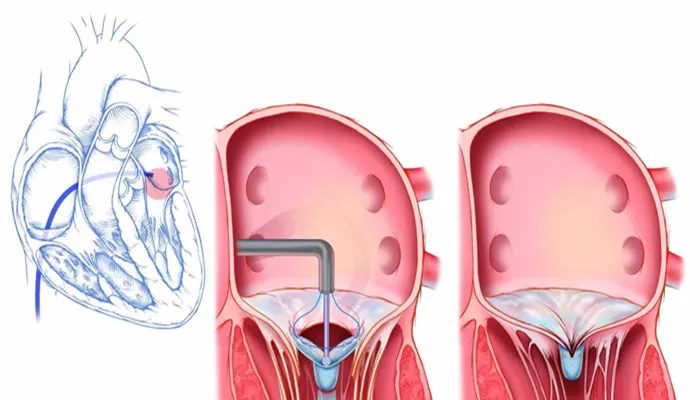
2. Surgical Repair or Replacement
For individuals with severe mitral regurgitation, surgery may be necessary to repair or replace the mitral valve. The type of surgery will depend on the extent of valve damage:
Mitral valve repair involves reshaping or repairing the existing valve to restore normal function.
Mitral valve replacement involves removing the damaged valve and replacing it with either a mechanical or biological valve.
3. Minimally Invasive Surgery
In some cases, minimally invasive surgical techniques, such as robotic surgery, may be used to repair or replace the mitral valve with smaller incisions, reducing recovery time.
4. Lifestyle Changes
Individuals with mitral regurgitation may be advised to make lifestyle changes, including:
- Maintaining a healthy weight
- Exercising regularly (as recommended by a doctor)
- Following a heart-healthy diet low in sodium and saturated fats
- Managing stress through relaxation techniques or counseling
Preventive Measures for Mitral Regurgitation
While some causes of mitral regurgitation, such as congenital defects, cannot be prevented, there are several measures that can help reduce the risk of developing the condition:
- Managing risk factors such as high blood pressure, high cholesterol, and diabetes
- Getting vaccinated to prevent infections like endocarditis
- Promptly treating infections such as strep throat to prevent rheumatic fever
- Regular heart check-ups for those at risk of heart disease
Conclusion
Mitral regurgitation is a serious heart condition that can lead to significant health problems if not properly managed.
Understanding the causes, symptoms, and treatment options is essential for individuals who may be at risk or have been diagnosed with the condition. Early detection and appropriate treatment can help prevent complications and improve the quality of life for those affected by mitral regurgitation. Regular medical check-ups and a heart-healthy lifestyle play a crucial role in managing and preventing this condition.
Related topics: