Torsades de Pointes (TdP) is a rare and potentially life-threatening type of abnormal heart rhythm, also known as arrhythmia. This condition is characterized by a rapid, irregular heartbeat that originates from the ventricles of the heart, and it typically results in a twisting or “twisting of the points” pattern on an electrocardiogram (ECG). TdP can cause the heart to beat inefficiently, impairing its ability to pump blood effectively and leading to symptoms such as dizziness, fainting, and even sudden cardiac arrest. It is a medical emergency that requires immediate intervention to prevent severe outcomes, including death.
While Torsades de Pointes is relatively uncommon, understanding its causes, symptoms, diagnosis, treatment, and management is crucial for clinicians and patients alike. In this article, we will explore these aspects in detail, providing a comprehensive overview of this dangerous condition.
Understanding Torsades De Pointes
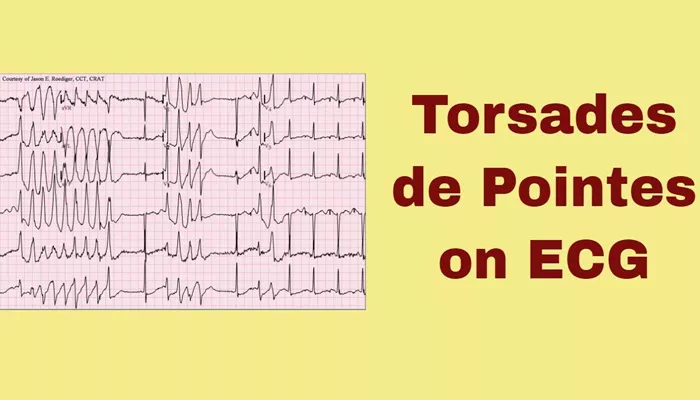
Torsades de Pointes is a specific form of polymorphic ventricular tachycardia (VT), meaning that it involves a rapid heart rate that originates in the ventricles, the lower chambers of the heart. What distinguishes TdP from other forms of VT is the characteristic “twisting” appearance of the QRS complexes on an ECG, which resembles a spindle-shaped or twisted pattern.
The term “torsades de pointes” is derived from the French words “torsades” (twists) and “pointes” (points), reflecting the dynamic nature of the ECG tracing during this arrhythmia.
The abnormal heart rhythm can be triggered by a variety of factors, including electrolyte imbalances, medications, congenital conditions, and other underlying cardiovascular diseases. TdP is often seen in patients with a prolonged QT interval, which is the time it takes for the heart’s electrical system to reset after each beat. A prolonged QT interval can increase the risk of TdP, and in many cases, it is a critical factor contributing to the development of this arrhythmia.
Causes of Torsades De Pointes
Torsades de Pointes can result from various causes that influence the heart’s electrical system. The most common factors that contribute to the development of TdP include:
1. Prolonged QT Interval
The most significant risk factor for TdP is a prolonged QT interval, which refers to a delay in the repolarization phase of the heart’s electrical cycle. A prolonged QT interval can be either congenital (present from birth) or acquired through various factors. Conditions that are associated with a prolonged QT interval include:
Congenital Long QT Syndrome (LQTS): A genetic disorder that affects the heart’s ion channels, leading to a prolonged QT interval. Several subtypes of LQTS exist, each associated with different genetic mutations.
Acquired Long QT Syndrome: A prolonged QT interval that develops later in life, often due to medications, electrolyte imbalances, or other underlying conditions.
2. Medications
Certain medications can cause or exacerbate a prolonged QT interval, increasing the risk of TdP. Some commonly implicated medications include:
Antiarrhythmic Drugs: Medications such as amiodarone, sotalol, and quinidine, which are used to treat arrhythmias, can prolong the QT interval and induce TdP.
Antibiotics: Some antibiotics, particularly macrolides (e.g., erythromycin) and fluoroquinolones (e.g., ciprofloxacin), can increase the risk of TdP.
Antidepressants: Tricyclic antidepressants (TCAs) and certain selective serotonin reuptake inhibitors (SSRIs) can prolong the QT interval.
Antipsychotic Medications: Drugs like haloperidol and ziprasidone, often used to manage psychiatric conditions, may also contribute to TdP.
3. Electrolyte Imbalances
Electrolytes, such as potassium, calcium, and magnesium, play a vital role in regulating the heart’s electrical activity.
Imbalances in these electrolytes can lead to a prolonged QT interval and increase the likelihood of TdP. Common electrolyte disturbances that can trigger TdP include:
Hypokalemia (low potassium): A decrease in potassium levels can lead to abnormal electrical impulses and increase the risk of arrhythmias, including TdP.
Hypomagnesemia (low magnesium): Magnesium is essential for stabilizing the heart’s electrical system. Low levels of magnesium can trigger TdP.
Hypocalcemia (low calcium): Calcium is crucial for the contraction of heart muscles. Low levels can contribute to prolonged QT intervals and TdP.
4. Heart Disease
Preexisting heart conditions can increase the risk of TdP, especially if they involve structural changes to the heart or affect the electrical conduction system. Conditions such as ischemic heart disease, heart failure, and cardiomyopathies (e.g., dilated or hypertrophic cardiomyopathy) can all lead to a higher risk of arrhythmias, including TdP.
5. Autonomic Nervous System Dysfunction
Imbalance in the autonomic nervous system, which controls involuntary functions such as heart rate and rhythm, can contribute to the onset of TdP. For example, excessive sympathetic nervous system activity (e.g., during stress or exercise) may trigger TdP in susceptible individuals.
Symptoms of Torsades De Pointes
The symptoms of TdP can range from mild to severe, depending on the duration and frequency of the arrhythmia. Some individuals may experience only occasional episodes of dizziness or palpitations, while others may experience more severe symptoms. Common symptoms include:
Palpitations: Patients often describe a racing or irregular heartbeat.
Dizziness or Lightheadedness: The heart’s inability to pump blood effectively can cause a drop in blood pressure, leading to dizziness or fainting.
Syncope (Fainting): A complete loss of consciousness can occur if the arrhythmia leads to insufficient blood flow to the brain.
Chest Pain: In some cases, TdP can be associated with chest discomfort or tightness due to inadequate blood flow to the heart.
Sudden Cardiac Arrest: If untreated, TdP can lead to a life-threatening situation known as sudden cardiac arrest, where the heart stops pumping blood effectively, resulting in death if not promptly treated.
Diagnosis of Torsades De Pointes
The diagnosis of Torsades de Pointes is typically made through an electrocardiogram (ECG), which records the electrical activity of the heart. The hallmark feature of TdP on an ECG is the characteristic “twisting” pattern of the QRS complexes, which resembles a spindle or twisted ribbon. The following steps are often involved in diagnosing TdP:
1. Electrocardiogram (ECG)
The ECG is the most important diagnostic tool for detecting TdP. The “twisting” pattern of the QRS complexes, as well as the prolonged QT interval, are indicative of TdP. An ECG will also help to identify other arrhythmias or underlying conditions that may be contributing to the arrhythmia.
2. Blood Tests
Blood tests may be performed to assess electrolyte levels, kidney function, and other biomarkers that may help identify the underlying causes of TdP. Tests for magnesium, potassium, and calcium are particularly important.
3. Holter Monitoring
In some cases, continuous ECG monitoring may be required to capture episodes of TdP that may not occur during a standard ECG. Holter monitors can record the heart’s electrical activity over a 24-hour period or longer.
4. Echocardiogram
An echocardiogram, which uses ultrasound waves to create images of the heart’s structure and function, may be used to rule out structural heart disease or assess the heart’s pumping ability.
Treatment of Torsades De Pointes
The treatment of TdP is focused on terminating the arrhythmia and addressing the underlying cause. In many cases, prompt intervention is required to prevent severe complications, such as sudden cardiac arrest. The main treatment options for TdP include:
1. Immediate Medical Intervention
Defibrillation: If the arrhythmia is causing significant symptoms, or if the patient has lost consciousness, electrical defibrillation may be required to reset the heart’s rhythm.
Magnesium Sulfate: Intravenous magnesium sulfate is often administered to correct any magnesium deficiency and stabilize the electrical activity of the heart.
Discontinuation of Triggering Medications: If a medication is found to be causing or exacerbating TdP, it must be immediately discontinued.
2. Correction of Electrolyte Imbalances
Potassium Replacement: If hypokalemia is present, potassium supplementation may be required to restore normal potassium levels.
Magnesium Replacement: If hypomagnesemia is identified, magnesium supplementation may be necessary to stabilize the heart’s electrical system.
Calcium Replacement: In cases of hypocalcemia, calcium supplementation may be used to correct the imbalance.
3. Long-Term Management
Once the immediate threat of TdP has been addressed, long-term management strategies may include:
Lifestyle Modifications: Avoidance of certain medications, managing stress, and maintaining a healthy lifestyle can help reduce the risk of recurrent episodes.
Implantable Cardioverter-Defibrillator (ICD): For patients with recurrent episodes or high risk of sudden cardiac arrest, an ICD may be implanted to deliver shocks to the heart if TdP or other dangerous arrhythmias occur.
Prevention of Torsades De Pointes
Prevention of TdP involves managing risk factors and addressing underlying conditions that contribute to the arrhythmia.
Key prevention strategies include:
Monitoring QT Interval: Patients on medications known to prolong the QT interval should be closely monitored with regular ECGs.
Electrolyte Management: Maintaining normal electrolyte levels, particularly potassium and magnesium, is essential for preventing TdP.
Avoiding Triggers: Patients should avoid substances or medications that can exacerbate TdP, such as drugs known to prolong the QT interval or cause electrolyte imbalances.
Conclusion
Torsades de Pointes is a serious and potentially fatal arrhythmia that requires prompt diagnosis and treatment. While the condition is relatively rare, understanding its causes, symptoms, and management strategies is essential for preventing adverse outcomes. Early recognition, correction of underlying issues, and appropriate treatment can significantly improve the prognosis for patients with TdP.
Related topics: