Obstructive sleep apnea (OSA) is a common sleep disorder characterized by repeated interruptions in breathing during sleep due to the obstruction of the upper airway. This condition affects millions of individuals worldwide and is associated with a multitude of health complications, including cardiovascular diseases. One of the lesser-discussed yet significant cardiovascular implications of OSA is its potential role in causing pulsational hypertension. This article delves into the relationship between obstructive sleep apnea and pulsational hypertension, exploring the mechanisms, symptoms, diagnosis, treatment options, and the broader implications for patient health.
Understanding Obstructive Sleep Apnea
Definition
Obstructive sleep apnea is defined by episodes of complete or partial obstruction of the upper airway during sleep, leading to reduced or paused airflow. These episodes can last from a few seconds to minutes and often result in arousals from sleep, leading to fragmented sleep and reduced overall sleep quality.
Causes
The primary causes of OSA include:
Anatomical Factors: Enlarged tonsils, a thick neck, or a narrow airway can contribute to airway obstruction during sleep.
Obesity: Excess body weight, particularly around the neck, increases the likelihood of airway collapse during sleep.
Age: The risk of OSA increases with age, as muscle tone in the throat decreases.
Gender: Men are more likely than women to develop OSA, although the risk in women increases after menopause.
Genetics: A family history of sleep apnea can increase susceptibility.
Symptoms
Common symptoms of OSA include:
Loud Snoring: Often reported by bed partners.
Choking or Gasping During Sleep: Witnessed by others.
Excessive Daytime Sleepiness: Resulting from poor sleep quality.
Fatigue: A general feeling of tiredness and lack of energy.
Morning Headaches: Due to increased intracranial pressure during episodes of apnea.
Difficulty Concentrating: Cognitive impairment can occur due to sleep deprivation.
Understanding Pulsational Hypertension
Definition
Pulsational hypertension, also known as pulsatile hypertension, refers to an increase in the amplitude of the blood pressure wave, characterized by elevated systolic blood pressure and a widening pulse pressure. This condition can indicate underlying cardiovascular issues and is often associated with increased arterial stiffness.
Causes
Pulsational hypertension can arise from various factors, including:
Increased Stroke Volume: Conditions that lead to increased blood volume or forceful contractions can raise systolic pressure.
Arterial Stiffness: Aging, atherosclerosis, and other conditions can lead to stiffer arteries, resulting in higher systolic pressure and lower diastolic pressure.
Increased Cardiac Output: Situations where the heart pumps more blood per minute, such as during exercise or stress.
Symptoms
Symptoms of pulsational hypertension may include:
Headaches: Often due to increased intracranial pressure.
Palpitations: Awareness of the heartbeat, particularly during episodes of high blood pressure.
Dizziness or Lightheadedness: Especially when blood pressure fluctuates significantly.
The Link Between Obstructive Sleep Apnea and Pulsational Hypertension
Mechanisms Linking OSA to Pulsational Hypertension
Intermittent Hypoxia: OSA is characterized by repeated episodes of oxygen desaturation during sleep. This intermittent hypoxia can lead to oxidative stress and inflammation, contributing to vascular dysfunction and increased arterial stiffness, both of which are risk factors for pulsational hypertension.
Sympathetic Nervous System Activation: The repeated arousals during apneic episodes activate the sympathetic nervous system, leading to increased heart rate and blood pressure. Chronic sympathetic activation can contribute to sustained hypertension and increased vascular resistance.
Endothelial Dysfunction: OSA has been associated with endothelial dysfunction, characterized by impaired vasodilation and increased vasoconstriction. This dysfunction can lead to increased vascular resistance and elevated systolic blood pressure.
Inflammation: OSA is associated with systemic inflammation, which can contribute to the development of hypertension. Elevated levels of inflammatory markers, such as C-reactive protein (CRP), have been observed in individuals with OSA.
Altered Hormonal Regulation: OSA can disrupt the normal regulation of hormones involved in blood pressure control, including renin, angiotensin, and aldosterone. These hormonal changes can lead to fluid retention and increased blood pressure.
Clinical Evidence
Numerous studies have examined the relationship between OSA and hypertension, revealing that:
Patients with OSA are at a significantly higher risk of developing hypertension compared to those without the condition.
The severity of OSA, as measured by the apnea-hypopnea index (AHI), correlates with the severity of hypertension.
Effective treatment of OSA, particularly with continuous positive airway pressure (CPAP) therapy, has been shown to improve blood pressure control in affected individuals.
Diagnosis of Pulsational Hypertension in the Context of OSA
Clinical Evaluation
Diagnosing pulsational hypertension in patients with OSA involves a comprehensive clinical evaluation, including:
Medical History: Gathering information on sleep patterns, symptoms of OSA, and family history of hypertension or cardiovascular disease.
Physical Examination: Assessing vital signs, including blood pressure measurements in different positions, and checking for signs of obesity or other risk factors.
Blood Pressure Measurement
Standard Blood Pressure Measurement: Blood pressure should be measured in a seated position after at least five minutes of rest. Pulsational hypertension is indicated by a high systolic blood pressure with a widened pulse pressure.
Ambulatory Blood Pressure Monitoring: Continuous monitoring can provide insights into blood pressure variability and help identify patterns of hypertension throughout the day.
Additional Diagnostic Tests
Polysomnography: This overnight sleep study is the gold standard for diagnosing OSA. It measures various parameters, including airflow, oxygen saturation, and sleep stages.
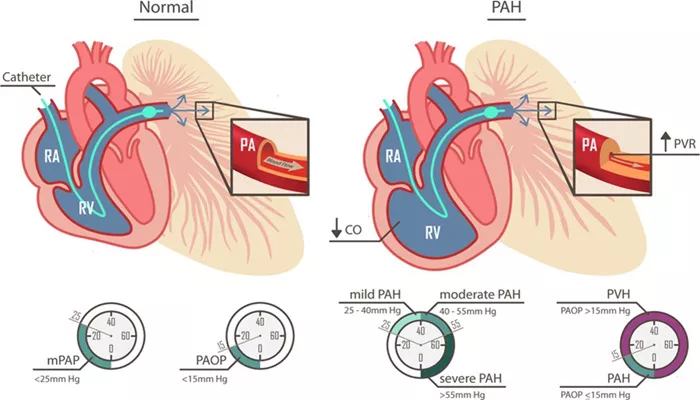
Echocardiography: This imaging test can assess right ventricular function and estimate pulmonary artery pressure, providing insights into the cardiovascular effects of OSA.
Blood Tests: Assessing levels of natriuretic peptides (e.g., BNP or NT-proBNP) can help confirm heart failure and evaluate its severity.
Arterial Stiffness Measurement: Techniques such as pulse wave velocity or arterial tonometry can assess arterial stiffness, providing additional context for pulsational hypertension.
Treatment of Obstructive Sleep Apnea and Pulsational Hypertension
Treatment of Obstructive Sleep Apnea
Continuous Positive Airway Pressure (CPAP): The most common and effective treatment for moderate to severe OSA, CPAP involves wearing a mask during sleep that delivers a continuous stream of air, keeping the airway open.
Lifestyle Modifications: Weight loss, positional therapy (sleeping on one’s side), and avoiding alcohol and sedatives can help reduce the severity of OSA.
Oral Appliances: Dental devices can help reposition the jaw and tongue to keep the airway open during sleep.
Surgery: In select cases, surgical interventions may be necessary to remove anatomical obstructions or correct structural issues contributing to OSA.
Management of Pulsational Hypertension
Pharmacological Interventions: If hypertension persists despite OSA treatment, antihypertensive medications may be necessary.
ACE Inhibitors: Help relax blood vessels and lower blood pressure.
Beta-Blockers: Reduce heart rate and improve cardiac output.
Calcium Channel Blockers: Help relax and widen blood vessels.
Diuretics: Help reduce fluid retention and lower blood pressure.
Lifestyle Modifications: Similar to OSA management, lifestyle changes such as dietary modifications, regular exercise, and weight management can help control blood pressure.
Monitoring and Follow-Up: Regular follow-up appointments are essential for monitoring blood pressure, assessing OSA symptoms, and adjusting treatment plans as necessary.
Implications for Patient Health
Quality of Life
The interplay between obstructive sleep apnea and pulsational hypertension can significantly impact a patient’s quality of life. Symptoms such as excessive daytime sleepiness, fatigue, and cognitive impairment can limit daily activities and social interactions. Effective management of both conditions is essential to improve overall well-being.
Long-Term Health Consequences
Untreated OSA and pulsational hypertension can lead to serious long-term health consequences, including:
Increased Risk of Cardiovascular Events: Patients with both conditions may be at higher risk for heart attacks, strokes, and other cardiovascular complications.
Worsening Heart Failure Symptoms: Poorly managed blood pressure can exacerbate heart failure symptoms, leading to a downward spiral of health deterioration.
Cognitive Impairment: Chronic hypertension and sleep deprivation are associated with an increased risk of cognitive decline and dementia. Effective management of both conditions is crucial to mitigating this risk.
Metabolic Syndrome: The combination of OSA and pulsational hypertension may contribute to the development of metabolic syndrome, increasing the risk of diabetes and other metabolic disorders.
Research and Future Directions
Ongoing research is essential to further elucidate the complex relationship between obstructive sleep apnea and pulsational hypertension. Areas of focus may include.
Mechanistic Studies: Investigating the underlying biological mechanisms linking OSA to pulsational hypertension and cardiovascular disease.
Longitudinal Studies: Assessing the long-term cardiovascular outcomes of patients with OSA and pulsational hypertension to better understand the trajectory of these conditions.
Intervention Studies: Evaluating the effectiveness of various treatment modalities for OSA and their impact on blood pressure control and overall cardiovascular health.
Conclusion
Obstructive sleep apnea is a prevalent condition that can lead to significant cardiovascular complications, including pulsational hypertension. The mechanisms linking OSA to pulsational hypertension involve a complex interplay of intermittent hypoxia, sympathetic nervous system activation, endothelial dysfunction, and systemic inflammation.
Recognizing the relationship between these two conditions is crucial for healthcare providers in diagnosing and managing affected patients. Through a combination of effective OSA treatment, lifestyle modifications, and careful management of blood pressure, healthcare providers can help mitigate the effects of both conditions and improve patient outcomes.
As our understanding of obstructive sleep apnea and its cardiovascular implications continues to evolve, it is vital to prioritize research, education, and awareness to enhance the management of patients suffering from these interconnected health issues. By doing so, we can work towards better health outcomes and improved quality of life for individuals affected by obstructive sleep apnea and pulsational hypertension.
Related Topics: