Heart failure is a serious medical condition that occurs when the heart is unable to pump blood effectively, leading to inadequate blood flow to meet the body’s needs. One form of heart failure is diastolic heart failure, also known as heart failure with preserved ejection fraction (HFpEF). Unlike systolic heart failure, where the heart’s ability to contract and pump blood is impaired, diastolic heart failure occurs when the heart’s ventricles lose the ability to relax and fill properly during the diastolic phase of the heartbeat. This leads to increased pressure within the heart and fluid buildup in the lungs and other areas of the body.
In this article, we will explore diastolic heart failure in detail, covering its causes, symptoms, and treatment options. Understanding the nature of this condition is critical for both patients and healthcare providers in managing the disease effectively and improving the quality of life.
What Is Diastolic Heart Failure?
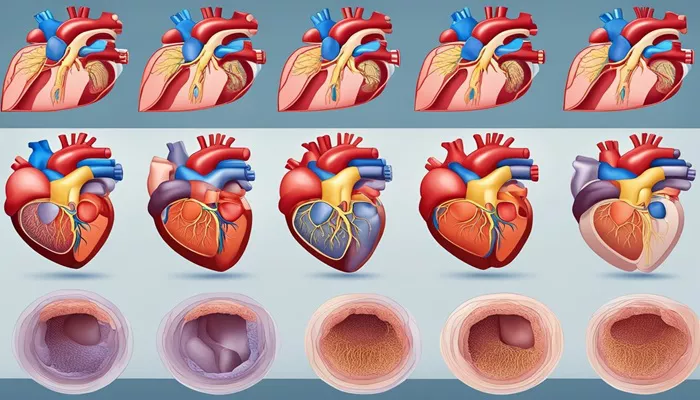
Diastolic heart failure refers to a condition in which the heart’s left ventricle, the chamber responsible for pumping oxygenated blood to the body, has become stiffened and less able to relax and fill with blood between heartbeats. In a healthy heart, the ventricles expand during the diastolic phase (the relaxation phase) to fill with blood before the next contraction. However, in individuals with diastolic heart failure, the left ventricle is stiff, reducing its capacity to fill properly. This results in inadequate blood flow and increased pressure within the heart, often leading to fluid accumulation in the lungs (pulmonary congestion) and other parts of the body.
Unlike systolic heart failure, where the heart’s pumping function is reduced, diastolic heart failure is characterized by a normal or near-normal ejection fraction. The ejection fraction is the percentage of blood that is pumped out of the left ventricle with each heartbeat. In diastolic heart failure, this percentage remains within the normal range, but the problem lies in the heart’s inability to properly fill with blood during diastole.
Causes of Diastolic Heart Failure
Several factors can contribute to the development of diastolic heart failure. In most cases, the condition is associated with other underlying heart diseases, including hypertension (high blood pressure), coronary artery disease, and diabetes. Let’s take a closer look at the major causes and risk factors:
1. Chronic High Blood Pressure (Hypertension)
Chronic high blood pressure is the most common cause of diastolic heart failure. Over time, elevated blood pressure causes the heart’s walls to thicken and become stiffer. This stiffening reduces the heart’s ability to relax and fill properly, leading to an increased risk of diastolic dysfunction. When the heart is unable to expand fully during diastole, the pressure within the heart rises, causing fluid buildup in the lungs and other areas of the body.
2. Coronary Artery Disease (CAD)
Coronary artery disease, which occurs when the arteries supplying blood to the heart become narrowed or blocked, can also lead to diastolic heart failure. Reduced blood flow to the heart muscle can cause it to become stiffened, impairing its ability to relax and fill with blood. Additionally, the presence of scar tissue from previous heart attacks can further reduce the flexibility of the heart muscle, leading to diastolic dysfunction.
3. Diabetes
Diabetes, particularly when poorly managed, is another significant risk factor for diastolic heart failure. High blood sugar levels over time can damage the blood vessels and contribute to the stiffening of the heart muscle. Moreover, diabetes often coexists with other conditions, such as hypertension and obesity, which further increase the risk of developing heart failure.
4. Aging
As people age, their heart muscle naturally becomes stiffer, making it more difficult for the ventricles to relax and fill during diastole. This age-related change can lead to diastolic heart failure, even in individuals without significant underlying heart disease. The risk of diastolic heart failure increases with age, particularly in individuals over 65.
5. Obesity
Obesity is another contributing factor to diastolic heart failure. Excess weight places added strain on the heart, leading to an increased risk of high blood pressure, diabetes, and coronary artery disease—all of which contribute to the development of diastolic dysfunction. Moreover, obesity can cause inflammation and other changes in the body that negatively impact heart function.
6. Other Causes and Risk Factors
Other less common causes of diastolic heart failure may include:
Valvular heart disease, where the heart’s valves do not function properly.
Cardiomyopathy, a condition in which the heart muscle becomes enlarged or stiffened due to inflammation or genetic factors.
Chronic kidney disease, which can contribute to fluid retention and high blood pressure.
Sleep apnea, a condition in which breathing is interrupted during sleep and may lead to high blood pressure and heart strain.
Symptoms of Diastolic Heart Failure
The symptoms of diastolic heart failure can vary in severity, depending on the extent of the heart’s dysfunction and how well the body is able to compensate for it. The most common symptoms of diastolic heart failure include:
1. Shortness of Breath (Dyspnea)
Shortness of breath, especially during physical exertion or while lying flat, is one of the hallmark symptoms of diastolic heart failure. As the heart becomes less efficient at filling with blood, fluid can accumulate in the lungs, leading to pulmonary congestion and difficulty breathing. This is often most noticeable during exercise or while at rest in a reclining position, a symptom known as orthopnea.
2. Fatigue
Individuals with diastolic heart failure often experience extreme fatigue or a feeling of being easily exhausted. This is due to the heart’s reduced ability to pump blood effectively, which leads to poor oxygen delivery to tissues and muscles, making it more difficult for individuals to engage in physical activities.
3. Swelling (Edema)
Swelling in the legs, ankles, or abdomen is another common symptom of diastolic heart failure. When the heart is unable to pump blood efficiently, fluid can build up in the body’s tissues, leading to swelling, also known as edema. This fluid buildup is particularly noticeable in the lower extremities and the abdomen.
4. Rapid or Irregular Heartbeat
In an attempt to compensate for the reduced efficiency of the heart, individuals with diastolic heart failure may experience an abnormal heart rhythm (arrhythmia). This can cause sensations of palpitations, where the heart seems to be racing or beating irregularly.
5. Coughing or Wheezing
Some individuals with diastolic heart failure may develop a persistent cough or wheezing, particularly at night or during periods of physical activity. This is often due to fluid buildup in the lungs, which can irritate the airways and lead to breathing difficulties.
6. Decreased Exercise Tolerance
Due to fatigue and shortness of breath, individuals with diastolic heart failure may find it difficult to exercise or perform physical activities that they were once able to do. Even mild exertion may cause symptoms to worsen.
Treatment of Diastolic Heart Failure
While there is currently no cure for diastolic heart failure, there are several treatment strategies that can help manage the condition, improve quality of life, and prevent further deterioration of heart function. Treatment typically focuses on controlling underlying conditions, reducing symptoms, and improving heart function.
1. Managing Underlying Conditions
Since many cases of diastolic heart failure are caused by chronic conditions such as high blood pressure, diabetes, and coronary artery disease, the first step in treatment is managing these conditions. Medications and lifestyle changes are often used to control blood pressure, regulate blood sugar, and reduce cholesterol levels.
Blood Pressure Control: Medications such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and beta-blockers are commonly used to lower blood pressure and reduce the strain on the heart.
Diabetes Management: Controlling blood sugar through diet, exercise, and medication is crucial to prevent further damage to the heart and blood vessels.
Cholesterol Management: Statins and other medications may be prescribed to lower cholesterol levels and prevent the progression of coronary artery disease.
2. Medications to Improve Heart Function
Although medications specifically designed to treat diastolic heart failure are limited, certain drugs can help relieve symptoms and improve heart function. These include:
Diuretics: Diuretics, or “water pills,” help reduce fluid buildup in the body by increasing urine production. This can help alleviate symptoms such as swelling and shortness of breath.
Aldosterone Antagonists: Medications like spironolactone can help reduce fluid retention and prevent further damage to the heart.
Calcium Channel Blockers: These medications can help relax the heart’s blood vessels, improving blood flow and reducing the stiffness of the heart muscle.
3. Lifestyle Modifications
Lifestyle changes play a critical role in managing diastolic heart failure. These modifications can help reduce the risk of complications and improve overall heart health. Key lifestyle recommendations include:
Diet: A heart-healthy diet that is low in sodium, saturated fats, and processed foods is essential for managing heart failure.
The DASH diet (Dietary Approaches to Stop Hypertension) is often recommended for individuals with high blood pressure and heart failure.
Exercise: Regular, moderate physical activity can help improve cardiovascular health and reduce symptoms. It is important to work with a healthcare provider to develop an appropriate exercise plan.
Weight Management: Maintaining a healthy weight is important, as excess weight can exacerbate symptoms and contribute to other risk factors such as high blood pressure and diabetes.
Avoiding Alcohol and Smoking: Limiting alcohol intake and avoiding smoking can help reduce the strain on the heart and improve overall cardiovascular health.
4. Advanced Therapies
In some cases, when symptoms are severe or other treatments are ineffective, more advanced therapies may be necessary.
These may include:
Cardiac Resynchronization Therapy (CRT): For some patients with advanced heart failure, a specialized pacemaker may be used to help coordinate the contractions of the heart’s ventricles and improve heart function.
Surgical Interventions: In certain cases, surgery may be required to repair or replace damaged heart valves or to treat coronary artery disease.
Conclusion
Diastolic heart failure is a chronic condition that affects the heart’s ability to relax and fill properly during the diastolic phase of the heartbeat. It can lead to fluid buildup in the lungs and other parts of the body, causing symptoms such as shortness of breath, fatigue, and swelling. The condition is often caused by underlying diseases such as hypertension, coronary artery disease, and diabetes. While there is no cure for diastolic heart failure, treatments are available to manage symptoms, address underlying conditions, and improve quality of life.
Related topics: