Myocardial inflammation, commonly known as myocarditis, is a condition characterized by inflammation of the heart muscle (myocardium). This inflammation can result from various etiological factors, including viral infections, autoimmune diseases, and exposure to toxins. While myocarditis can present with a range of symptoms, one of the most common and significant symptoms is chest pain. This article will explore myocardial inflammation in detail, focusing on its causes, clinical manifestations, diagnostic methods, and management strategies, with a particular emphasis on chest pain as a prevalent symptom.
Understanding Myocardial Inflammation
Definition of Myocarditis
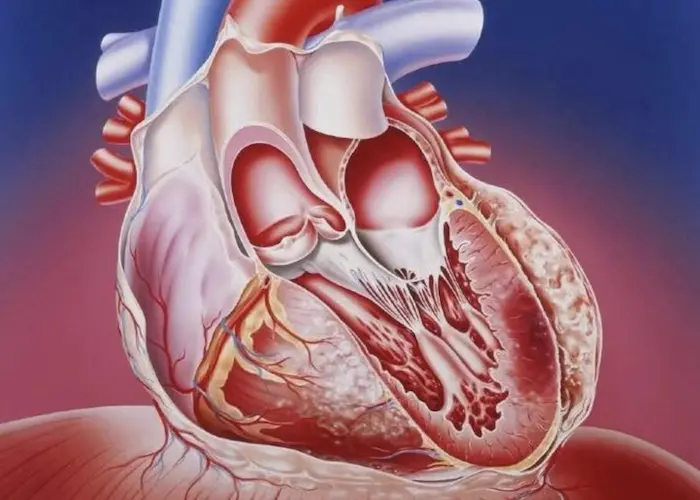
Myocarditis is defined as an inflammatory condition affecting the myocardium, the muscular layer of the heart wall. The inflammation can lead to structural damage, electrical instability, and impaired cardiac function. The condition can present acutely or chronically and may lead to significant morbidity and mortality if not recognized and treated promptly.
Causes of Myocarditis
Myocarditis can result from various etiological factors, which can be broadly categorized into infectious and non-infectious causes:
Infectious Causes:
Viral Infections: The most common infectious cause of myocarditis is viral infections, particularly those caused by enteroviruses (e.g., Coxsackievirus), adenoviruses, and parvovirus B19. These viruses can directly invade myocardial cells, leading to inflammation and damage.
Bacterial Infections: Bacterial pathogens such as Borrelia burgdorferi (Lyme disease) and Streptococcus can also lead to myocarditis. In rare cases, myocarditis can be caused by bacterial toxins or post-infectious immune reactions.
Fungal and Parasitic Infections: Less frequently, myocarditis can result from fungal infections (e.g., histoplasmosis) and parasitic infections such as Chagas disease (Trypanosoma cruzi).
Non-Infectious Causes:
Autoimmune Diseases: Conditions like systemic lupus erythematosus (SLE) and rheumatoid arthritis can lead to myocarditis due to immune-mediated damage to myocardial tissue.
Toxins: Exposure to certain drugs (e.g., cocaine, some chemotherapy agents) and alcohol can result in myocardial inflammation.
Idiopathic: In some cases, the exact cause of myocarditis remains unknown, despite thorough investigation.
Symptoms of Myocarditis
Myocarditis can present with a variety of symptoms, which may vary in severity and duration. The most common symptoms include.
Chest Pain: Often described as sharp, pressure-like, or squeezing. This is typically the most significant and prevalent symptom of myocarditis.
Shortness of Breath: Patients may experience difficulty breathing during exertion or at rest, which can be indicative of heart failure.
Fatigue: A general feeling of weakness or tiredness is common, especially in the presence of heart failure or reduced cardiac output.
Palpitations: Patients may report irregular heartbeats or a sensation of a racing heart, often linked to arrhythmias.
Fever: Particularly in cases of infectious myocarditis, patients may present with fever and other systemic symptoms.
The Role of Chest Pain in Myocardial Inflammation
Understanding Chest Pain
Chest pain is a common symptom that can arise from various cardiovascular and non-cardiovascular conditions. In the context of myocarditis, chest pain may be due to.
Myocardial Ischemia: Inflammation can lead to impaired blood flow to the heart muscle, resulting in ischemic chest pain.
Pericardial Involvement: In some cases, myocarditis may also involve the pericardium (the fibrous sac surrounding the heart), leading to pericarditis, which can cause sharp, pleuritic chest pain that worsens with deep breathing.
Direct Inflammation: Inflammatory mediators released during myocarditis can sensitize nerve endings in the myocardium, leading to pain.
Characteristics of Chest Pain in Myocarditis
The characteristics of chest pain associated with myocarditis can vary, but common features include:
Quality: Patients may describe the pain as sharp, stabbing, or pressure-like.
Location: The pain is often retrosternal (behind the breastbone) but can radiate to the shoulders, arms, neck, or back.
Duration: Chest pain may be persistent or intermittent, lasting from minutes to hours.
Associated Symptoms: Chest pain in myocarditis may be accompanied by other symptoms, such as shortness of breath, palpitations, or fatigue.
Differential Diagnosis of Chest Pain
When evaluating a patient with chest pain, it is essential to consider other potential causes. Differential diagnoses include.
Acute Coronary Syndrome (ACS): Myocarditis can mimic the presentation of ACS, including unstable angina and myocardial infarction. However, troponin levels may be significantly elevated in both conditions.
Pericarditis: Inflammation of the pericardium can cause chest pain that may be sharp and worsens with deep breathing or lying flat.
Pulmonary Embolism: This condition can present with sudden onset chest pain and shortness of breath, necessitating prompt evaluation.
Gastroesophageal Reflux Disease (GERD): Reflux can cause chest discomfort that mimics cardiac pain, often associated with heartburn or regurgitation.
Diagnostic Evaluation of Myocarditis
Clinical History and Physical Examination
A thorough clinical history and physical examination are essential for diagnosing myocarditis. Key elements to assess include.
Symptom Onset and Duration: Understanding the timeline of symptoms can help differentiate acute from chronic myocarditis.
Past Medical History: A history of recent viral infections, autoimmune diseases, or exposure to toxins can provide clues to the underlying cause.
Physical Examination: Signs of heart failure (e.g., elevated jugular venous pressure, crackles on lung auscultation) and arrhythmias may be noted during the examination.
Laboratory Tests
Laboratory tests play a crucial role in diagnosing myocardial inflammation. Specific markers include.
Cardiac Biomarkers
Troponin I and T: Elevated levels of cardiac troponins are highly specific for myocardial injury and can indicate myocardial inflammation. Troponin levels may be significantly elevated in acute myocarditis, reflecting myocardial damage.
Creatine Kinase (CK) and CK-MB: These enzymes may also be elevated in myocarditis, although they are less specific than troponins.
Inflammatory Markers
C-Reactive Protein (CRP): Elevated CRP levels indicate systemic inflammation and may be observed in myocarditis.
Erythrocyte Sedimentation Rate (ESR): An elevated ESR can also suggest inflammation but is nonspecific.
Viral Serologies
In cases of suspected viral myocarditis, specific viral serologies may be performed to identify the causative agent. For example, testing for antibodies against Coxsackievirus or parvovirus B19 can provide diagnostic clues.
Imaging Studies
Imaging modalities are essential for assessing myocardial inflammation and its effects on cardiac structure and function.
Echocardiography
Echocardiography is a non-invasive imaging technique that can help evaluate cardiac function and detect wall motion abnormalities. Key findings in myocarditis may include.
Left Ventricular Dysfunction: Systolic or diastolic dysfunction may be observed.
Regional Wall Motion Abnormalities: These may occur due to localized inflammation or ischemia.
Cardiac Magnetic Resonance Imaging (MRI)
Cardiac MRI is a highly sensitive and specific tool for diagnosing myocarditis. It can provide detailed information about myocardial inflammation and fibrosis. Specific MRI findings in myocarditis include.
Myocardial Edema: Increased signal intensity on T2-weighted images indicates edema, a hallmark of inflammation.
Late Gadolinium Enhancement: This finding suggests myocardial scarring or fibrosis, which may occur in chronic myocarditis.
Positron Emission Tomography (PET)
PET imaging can be used to assess myocardial inflammation by evaluating metabolic activity. Increased uptake of radiotracers in the myocardium may indicate active inflammation.
Electrocardiogram (ECG) Changes
The ECG is a valuable tool for diagnosing myocardial inflammation. Specific ECG changes associated with myocarditis include.
ST Segment Changes
ST Segment Elevation: This may occur in acute myocarditis, resembling ST-elevation myocardial infarction (STEMI).
ST Segment Depression: This may indicate subendocardial ischemia or increased myocardial demand.
T Wave Changes
T Wave Inversion: Inverted T waves may be observed in the context of myocardial injury and inflammation.
T Wave Flattening: Flattened T waves may indicate electrolyte imbalances or autonomic dysregulation.
Arrhythmias
Arrhythmias are common in myocarditis and can manifest as:
Atrial Fibrillation: Due to atrial enlargement or increased pressure.
Ventricular Tachycardia: In severe cases, indicating significant myocardial damage.
QRS Complex Changes
Prolonged QRS Duration: This may suggest conduction abnormalities resulting from inflammation.
Pathological Q Waves: These may develop in the setting of myocardial necrosis.
Management of Myocardial Inflammation
Supportive Care
Management of myocarditis often begins with supportive care, which may include:
Monitoring: Patients should be closely monitored for changes in symptoms, heart function, and arrhythmias.
Rest: Reducing physical activity may help minimize stress on the heart during the acute inflammatory phase.
Pharmacological Management
The treatment of myocardial inflammation may involve various pharmacological interventions:
Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to reduce inflammation and relieve symptoms.
Immunosuppressive Therapy: In cases of autoimmune myocarditis, corticosteroids or other immunosuppressive agents may be indicated.
Heart Failure Management: Patients with heart failure symptoms may require medications such as diuretics, ACE inhibitors, and beta-blockers to optimize cardiac function.
Antiviral Therapy: In cases of viral myocarditis, antiviral medications may be considered, although their efficacy is variable.
Advanced Interventions
In severe cases of myocarditis with significant heart failure or arrhythmias, advanced interventions may be necessary:
Mechanical Circulatory Support: In cases of acute heart failure, devices such as intra-aortic balloon pumps or ventricular assist devices may be used.
Heart Transplantation: For patients with end-stage heart failure due to myocarditis, heart transplantation may be considered.
Prognosis and Long-Term Management
Prognosis
The prognosis for patients with myocarditis can vary widely based on several factors:
Severity of Inflammation: More severe inflammation and myocardial damage are associated with worse outcomes.
Timeliness of Diagnosis and Treatment: Early recognition and appropriate management can improve prognosis and reduce the risk of complications.
Underlying Cause: The underlying cause of myocarditis can influence long-term outcomes. For example, viral myocarditis may have a better prognosis than autoimmune-related myocarditis.
Long-Term Management
Patients recovering from myocarditis should be monitored for potential long-term complications, including:
Heart Failure: Some patients may develop chronic heart failure, requiring ongoing management and follow-up.
Arrhythmias: Patients should be evaluated for the risk of arrhythmias, and those with significant arrhythmias may require further intervention.
Cardiac Rehabilitation: A structured cardiac rehabilitation program can help improve exercise capacity and overall cardiovascular health.
Conclusion
Chest pain is the most common symptom of myocardial inflammation, or myocarditis, and serves as a critical indicator of the underlying condition. Understanding the characteristics, differential diagnoses, and associated symptoms of chest pain is essential for timely diagnosis and management of myocarditis.
In addition to chest pain, patients may present with a range of symptoms, including shortness of breath, fatigue, palpitations, and fever. A comprehensive diagnostic approach, including clinical evaluation, laboratory tests, imaging studies, and ECG changes, is necessary to confirm the diagnosis and guide appropriate management.
Effective management of myocarditis involves supportive care, pharmacological interventions, and, in severe cases, advanced therapies. Early recognition and treatment are crucial for improving prognosis and reducing the risk of complications.
Related Topics: