Heart Failure with Preserved Ejection Fraction (HFpEF) is a complex and increasingly prevalent form of heart failure that presents unique challenges in diagnosis and management. Understanding whether HFpEF is classified as diastolic or systolic heart failure is crucial for both healthcare providers and patients. This article will explore the characteristics of HFpEF, its pathophysiology, distinguishing features from other forms of heart failure, diagnostic criteria, treatment options, and the implications of its classification as diastolic heart failure.
Understanding Heart Failure
What is Heart Failure
Heart failure (HF) is a clinical syndrome that arises when the heart is unable to pump blood effectively to meet the body’s needs. This can result in a variety of symptoms, including shortness of breath, fatigue, fluid retention, and decreased exercise tolerance. Heart failure can be classified into two main categories based on the heart’s ejection fraction (EF):
Heart Failure with Reduced Ejection Fraction (HFrEF): Characterized by an EF of less than 40%, HFrEF occurs when the heart’s ability to contract and pump blood is impaired. This is often due to conditions such as coronary artery disease, myocardial infarction, or dilated cardiomyopathy.
Heart Failure with Preserved Ejection Fraction (HFpEF): In contrast, HFpEF is defined by a normal EF (typically 50% or greater) but involves impaired filling of the heart during diastole. This condition is often associated with a range of comorbidities, including hypertension, obesity, diabetes, and atrial fibrillation.
Diastolic vs. Systolic Heart Failure
To understand HFpEF, it is essential to differentiate between diastolic and systolic heart failure:
Diastolic Heart Failure: This refers to heart failure characterized by impaired relaxation of the heart muscle during diastole (the filling phase). In diastolic heart failure, the heart can contract normally, but it cannot fill adequately due to stiffness or other abnormalities in the heart muscle. HFpEF falls into this category.
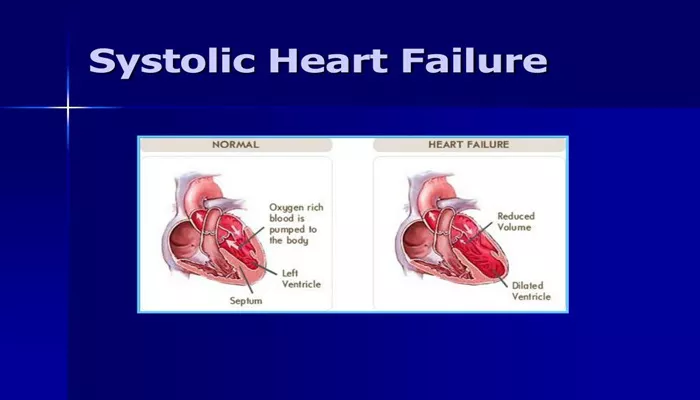
Systolic Heart Failure: This type of heart failure occurs when the heart’s ability to contract and eject blood is compromised. In systolic heart failure, the heart muscle is weakened, leading to reduced ejection fraction and impaired cardiac output.
The Pathophysiology of HFpEF
Mechanisms of Diastolic Dysfunction
HFpEF is primarily characterized by diastolic dysfunction, which can result from various underlying mechanisms:
Ventricular Stiffness: Increased stiffness of the left ventricle can impede its ability to relax during diastole, leading to elevated filling pressures. This stiffness may be due to hypertrophy (thickening) of the heart muscle, often caused by chronic hypertension.
Impaired Relaxation: The heart muscle may have difficulty relaxing properly due to various factors, including ischemia, fibrosis, and changes in the extracellular matrix.
Increased Left Atrial Pressure: As the left ventricle becomes less compliant, pressure can build up in the left atrium, leading to atrial enlargement and the development of atrial fibrillation.
Comorbid Conditions: Conditions such as obesity, diabetes, and chronic kidney disease can contribute to the development of diastolic dysfunction and HFpEF.
Clinical Consequences
The pathophysiological changes associated with HFpEF can lead to a range of clinical consequences:
Pulmonary Congestion: Elevated left atrial pressures can result in fluid accumulation in the lungs, leading to symptoms such as shortness of breath, especially during exertion or when lying flat.
Exercise Intolerance: Patients with HFpEF often experience decreased exercise capacity due to impaired cardiac output and increased heart rate response during physical activity.
Fatigue: The inability of the heart to meet the body’s demands can lead to fatigue and reduced quality of life.
Characteristics of HFpEF
Symptoms
Patients with HFpEF may present with a variety of symptoms, including:
Dyspnea: Shortness of breath, particularly during exertion or at rest, is a hallmark symptom of HFpEF.
Fatigue: Patients often report significant fatigue and decreased exercise tolerance.
Edema: Fluid retention can lead to swelling in the legs, ankles, and abdomen.
Palpitations: Atrial fibrillation is common in patients with HFpEF and can contribute to symptoms of palpitations.
Risk Factors
Several risk factors are associated with the development of HFpEF:
Hypertension: Chronic high blood pressure is the most significant risk factor for HFpEF, leading to ventricular hypertrophy and stiffness.
Obesity: Excess body weight is linked to increased cardiac workload and can contribute to the development of HFpEF.
Diabetes: Diabetes mellitus is associated with metabolic changes that can lead to heart muscle stiffness and diastolic dysfunction.
Age: HFpEF is more prevalent in older adults, with age-related changes in cardiac structure and function contributing to its development.
Coronary Artery Disease: Ischemic heart disease can contribute to HFpEF through myocardial damage and remodeling.
Diagnosis of HFpEF
Clinical Evaluation
Diagnosing HFpEF involves a comprehensive clinical evaluation, including:
Medical History: A thorough medical history helps identify risk factors, comorbidities, and symptoms.
Physical Examination: A physical examination may reveal signs of fluid retention, elevated jugular venous pressure, and abnormal lung sounds.
Diagnostic Tests
Several diagnostic tests are commonly used to confirm the diagnosis of HFpEF:
Electrocardiogram (ECG): An ECG can identify arrhythmias, previous myocardial infarctions, and other cardiac abnormalities.
Echocardiography: This imaging technique provides information about cardiac structure and function, helping to assess ejection fraction and diastolic function. Key parameters evaluated include left ventricular hypertrophy, left atrial size, and diastolic filling patterns.
Chest X-ray: A chest X-ray can reveal signs of heart enlargement and pulmonary congestion.
Blood Tests: Blood tests, including B-type natriuretic peptide (BNP) levels, can help assess heart failure severity and identify potential underlying causes.
Diagnostic Criteria
The diagnosis of HFpEF is typically made based on the following criteria:
Symptoms of Heart Failure: Patients must exhibit symptoms consistent with heart failure, such as dyspnea, fatigue, and fluid retention.
Preserved Ejection Fraction: An echocardiogram must demonstrate an ejection fraction of 50% or greater.
Evidence of Diastolic Dysfunction: Echocardiographic findings indicating impaired diastolic function, such as elevated left atrial pressure or abnormal filling patterns, are necessary to confirm the diagnosis.
Treatment Strategies for HFpEF
The management of HFpEF is multifaceted and aims to alleviate symptoms, improve quality of life, and reduce hospitalizations. While there is no specific treatment proven to improve mortality in HFpEF, several strategies can be employed to manage the condition effectively.
Lifestyle Modifications
Lifestyle changes play a crucial role in managing HFpEF and can significantly improve symptoms and overall health.
Dietary Changes
Low-Sodium Diet: Reducing sodium intake can help manage fluid retention and lower blood pressure. Patients are typically advised to limit sodium to less than 2,000 mg per day.
Heart-Healthy Diet: A diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support cardiovascular health. The Mediterranean diet is often recommended for its heart-protective benefits.
Weight Management: Achieving and maintaining a healthy weight can reduce the heart’s workload and improve symptoms.
Physical Activity
Regular Exercise: Engaging in regular physical activity, as tolerated, can improve cardiovascular fitness and reduce symptoms of heart failure. Patients should work with their healthcare provider to develop a safe exercise plan tailored to their abilities.
Cardiac Rehabilitation: Structured cardiac rehabilitation programs can provide supervised exercise training, education, and support to help patients manage their condition.
Smoking Cessation and Alcohol Moderation
Quit Smoking: Smoking cessation is crucial for improving heart health and reducing the risk of cardiovascular complications.
Limit Alcohol Intake: Excessive alcohol consumption can worsen heart failure symptoms and should be limited.
Pharmacological Treatments
While there is no specific medication approved for HFpEF, several classes of drugs can help manage symptoms and improve outcomes.
Diuretics
Loop Diuretics: Medications such as furosemide (Lasix) and bumetanide are commonly used to relieve fluid retention and reduce symptoms of congestion. They help promote urine production and decrease edema.
Antihypertensive Medications
ACE Inhibitors: Angiotensin-converting enzyme (ACE) inhibitors, such as lisinopril and ramipril, can help lower blood pressure and improve heart function by reducing afterload.
Angiotensin II Receptor Blockers (ARBs): ARBs, such as losartan and valsartan, may be used as alternatives to ACE inhibitors, particularly in patients who cannot tolerate them.
Beta-Blockers: These medications, including metoprolol and carvedilol, can help manage heart rate and blood pressure, improving overall heart function.
Calcium Channel Blockers: Dihydropyridine calcium channel blockers, such as amlodipine, can be used to manage hypertension, but non-dihydropyridine agents should be used cautiously due to their potential effects on heart rate.
Aldosterone Antagonists
Spironolactone and Eplerenone: These medications can help manage fluid retention and have been shown to improve outcomes in some patients with HFpEF, particularly those with concurrent hypertension.
SGLT2 Inhibitors
Empagliflozin and Dapagliflozin: Sodium-glucose cotransporter-2 (SGLT2) inhibitors, originally developed for diabetes management, have shown promise in reducing heart failure hospitalizations and improving outcomes in patients with HFpEF. They work by promoting diuresis and reducing the risk of fluid overload.
Other Medications
Digoxin: While not commonly used for HFpEF, digoxin may be considered in patients with atrial fibrillation and heart failure to help control heart rate.
Vasodilators: In some cases, medications that dilate blood vessels, such as nitrates, may be used to relieve symptoms of congestion.
Management of Comorbidities
Effective management of comorbid conditions is essential in patients with HFpEF. Addressing underlying issues can significantly improve heart failure symptoms and overall health.
Hypertension Management
Blood Pressure Control: Maintaining optimal blood pressure levels is critical for patients with HFpEF. Regular monitoring and adherence to antihypertensive medications can help achieve this goal.
Diabetes Management
Glycemic Control: Patients with diabetes should work closely with their healthcare provider to achieve optimal blood sugar levels, as uncontrolled diabetes can worsen heart failure.
Management of Atrial Fibrillation
Rate Control: In patients with atrial fibrillation, controlling heart rate through medications such as beta-blockers or calcium channel blockers is essential for improving symptoms and reducing the risk of complications.
Emerging Therapies and Research
Research is ongoing to identify new treatment options for HFpEF, including:
Novel Pharmacological Agents
Natriuretic Peptides: Investigational therapies targeting natriuretic peptides aim to improve diuresis and reduce congestion in HFpEF patients.
Soluble Guanylate Cyclase Stimulators: These agents are being studied for their potential to improve cardiac function and reduce symptoms in HFpEF.
Inflammation Modulators: Given the role of inflammation in HFpEF, therapies targeting inflammatory pathways are being explored.
Gene Therapy and Regenerative Medicine
Stem Cell Therapy: Research into the use of stem cells to regenerate damaged heart tissue and improve function is ongoing.
Gene Editing: Advances in gene therapy may offer future treatment options for patients with genetic predispositions to heart failure.
Conclusion
Heart Failure with Preserved Ejection Fraction (HFpEF) is classified as a form of diastolic heart failure due to its primary characteristic of impaired diastolic filling despite a preserved ejection fraction. Understanding the pathophysiology, symptoms, diagnosis, and treatment options for HFpEF is essential for healthcare providers and patients alike.
While HFpEF presents unique challenges, a comprehensive management approach that includes lifestyle modifications, pharmacological treatments, and the management of comorbid conditions can significantly improve the quality of life for affected individuals. Ongoing research into novel therapies and a better understanding of the underlying mechanisms of HFpEF will continue to shape the future of its management. By prioritizing patient education and adherence to treatment plans, we can empower individuals to take an active role in managing their health and navigating the complexities of heart failure with preserved ejection fraction.
Related Topics: