Congestive heart failure (CHF) is a chronic and progressive condition in which the heart is unable to pump sufficient blood to meet the body’s needs. This condition can lead to a range of symptoms, including shortness of breath, fatigue, and fluid retention. While CHF is a serious diagnosis, many individuals can manage the condition effectively and maintain a good quality of life for many years. This article explores the factors that influence life expectancy in individuals with CHF, the stages of the disease, treatment options, and lifestyle modifications that can help improve outcomes.
Understanding Congestive Heart Failure
Definition of Congestive Heart Failure
Congestive heart failure is a condition characterized by the heart’s inability to pump blood effectively. It can affect one or both sides of the heart and is often the result of other underlying conditions such as coronary artery disease, hypertension, or previous heart attacks. CHF can be classified into two main types:
Systolic Heart Failure: This occurs when the heart muscle becomes weak and cannot contract effectively, leading to reduced ejection fraction (the amount of blood pumped out of the heart with each beat).
Diastolic Heart Failure: In this type, the heart muscle becomes stiff and cannot relax properly, leading to impaired filling of the heart chambers.
Causes of Congestive Heart Failure
Several factors can contribute to the development of CHF, including:
Coronary Artery Disease: The most common cause of CHF, where the arteries supplying blood to the heart become narrowed or blocked.
High Blood Pressure: Chronic hypertension can lead to thickening of the heart muscle, reducing its efficiency.
Heart Attack: Damage to the heart muscle from a heart attack can impair its ability to pump effectively.
Valvular Heart Disease: Malfunctioning heart valves can disrupt normal blood flow and lead to CHF.
Cardiomyopathy: Diseases of the heart muscle, whether due to genetic factors, alcohol abuse, or infections, can lead to CHF.
Arrhythmias: Abnormal heart rhythms can affect the heart’s ability to pump blood efficiently.
Other Conditions: Conditions such as diabetes, obesity, and thyroid disorders can also increase the risk of developing CHF.
Symptoms of Congestive Heart Failure
Symptoms of CHF can vary in severity and may include:
Shortness of Breath: This can occur during exertion or while lying down (orthopnea).
Fatigue: Individuals may experience extreme tiredness due to the heart’s reduced ability to pump blood.
Fluid Retention: Swelling in the legs, ankles, and abdomen can occur due to fluid buildup.
Rapid or Irregular Heartbeat: Patients may notice palpitations or a racing heart.
Persistent Cough or Wheezing: Fluid accumulation in the lungs can lead to respiratory symptoms.
Decreased Exercise Tolerance: Individuals may find it difficult to engage in physical activities they once enjoyed.
Stages of Congestive Heart Failure
CHF is typically classified into four stages, which help determine the severity of the condition and guide treatment:
Stage A: At Risk
Individuals in Stage A are at high risk for developing heart failure but do not have any structural heart disease or symptoms.
Risk factors may include hypertension, diabetes, obesity, and a family history of heart disease.
Stage B: Structural Heart Disease
In Stage B, individuals have structural heart disease but do not exhibit symptoms of heart failure. This may include conditions such as previous heart attacks or valvular heart disease.
Stage C: Symptomatic Heart Failure
Stage C is characterized by the presence of symptoms of heart failure, such as shortness of breath and fatigue. Patients may experience limitations in physical activity and may have reduced exercise tolerance.
Stage D: Advanced Heart Failure
Individuals in Stage D have advanced heart failure with severe symptoms that may not respond well to treatment. Patients may require specialized interventions, such as heart transplantation or mechanical support devices.
Life Expectancy with Congestive Heart Failure
Factors Influencing Life Expectancy
The life expectancy of individuals with CHF can vary significantly based on several factors, including:
Severity of the Condition: The stage of heart failure plays a crucial role in determining prognosis. Patients in earlier stages (A and B) typically have a better outlook than those in advanced stages (C and D).
Underlying Causes: The presence of other medical conditions, such as diabetes, kidney disease, or chronic obstructive pulmonary disease (COPD), can negatively impact life expectancy.
Response to Treatment: How well a patient responds to treatment, including medications and lifestyle modifications, can influence outcomes.
Age and Gender: Generally, younger patients tend to have a better prognosis than older individuals. Additionally, studies have shown that women may have a slightly better prognosis than men.
Comorbid Conditions: The presence of additional health issues can complicate the management of CHF and affect life expectancy.
Statistical Insights
While it is difficult to provide a definitive answer regarding life expectancy in CHF patients, some studies have provided insights.
General Statistics: According to the American Heart Association, about 50% of individuals diagnosed with heart failure will survive more than five years. However, this varies widely based on the severity of the disease and individual health factors.
Median Survival: Research indicates that the median survival for patients with heart failure ranges from 1 to 5 years, with some studies suggesting that approximately 30% of patients may survive for 10 years or more.
Prognostic Models: Various prognostic models, such as the Seattle Heart Failure Model, can help estimate life expectancy based on clinical factors, including age, gender, ejection fraction, and comorbidities.
Quality of Life Considerations
While life expectancy is an important aspect of living with CHF, quality of life is equally significant. Many individuals with CHF can manage their symptoms effectively and maintain a good quality of life through:
Effective Symptom Management: Proper management of symptoms can lead to improved daily functioning and well-being.
Supportive Care: Access to healthcare providers, support groups, and counseling can enhance emotional and psychological well-being.
Lifestyle Modifications: Adopting a heart-healthy lifestyle can improve overall health and well-being.
Treatment Options for Congestive Heart Failure
Medical Management
The management of CHF typically involves a combination of lifestyle changes and medications:
Medications: Commonly prescribed medications include:
ACE Inhibitors: Help relax blood vessels and lower blood pressure.
Beta-Blockers: Reduce heart rate and improve heart function.
Diuretics: Help reduce fluid retention and alleviate symptoms.
Aldosterone Antagonists: Help manage fluid balance and improve outcomes in heart failure.
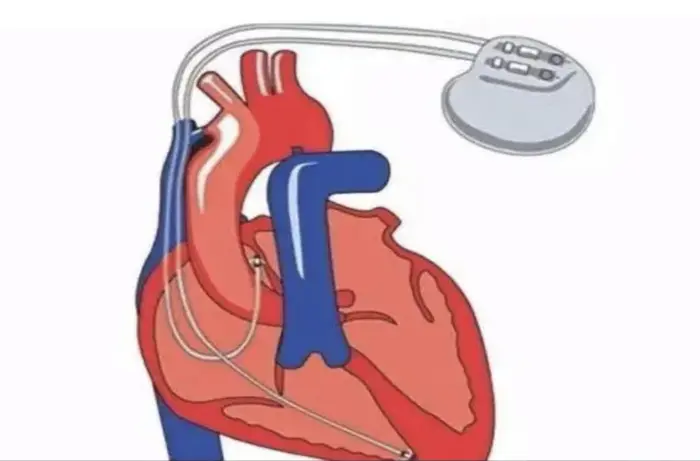
Device Therapy: In some cases, device therapy may be indicated:
Implantable Cardioverter-Defibrillator (ICD): For patients at high risk of life-threatening arrhythmias.
Cardiac Resynchronization Therapy (CRT): Improves heart function in patients with electrical conduction abnormalities.
Heart Transplantation: For eligible patients with advanced heart failure who do not respond to other treatments, heart transplantation may be considered.
Lifestyle Modifications
Making lifestyle changes is essential for managing CHF and improving outcomes:
Dietary Changes: Following a heart-healthy diet, such as the DASH diet, can help manage symptoms and reduce fluid retention. This includes:
Reducing sodium intake.
Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins.
Regular Exercise: Engaging in regular physical activity, as advised by a healthcare provider, can improve cardiovascular fitness and overall well-being.
Weight Management: Maintaining a healthy weight can reduce the strain on the heart.
Avoiding Alcohol and Smoking: Quitting smoking and limiting alcohol intake can significantly benefit heart health.
Stress Management: Techniques such as meditation, yoga, and deep breathing exercises can help reduce stress and improve quality of life.
Living with Congestive Heart Failure
Managing Daily Life
Living with CHF requires ongoing management and adjustments to daily activities. Key strategies include.
Regular Follow-Up Care: Regular appointments with healthcare providers are essential for monitoring heart function and adjusting treatment plans as needed.
Education and Awareness: Understanding the condition and its management can empower patients to take an active role in their health.
Support Systems: Building a support network of family, friends, and healthcare providers can provide emotional support and practical assistance in managing the condition.
Adjusting Activities
Individuals with CHF may need to adjust their activities to accommodate their condition. This may include.
Pacing Activities: Learning to pace oneself and recognizing limits can help prevent fatigue and shortness of breath.
Avoiding Intense Physical Exertion: While regular exercise is important, individuals with CHF should avoid activities that are excessively strenuous or may trigger symptoms.
Monitoring Symptoms: Keeping track of symptoms and any changes in health can help individuals and their healthcare providers make informed decisions about treatment and lifestyle adjustments.
Psychological Impact
Living with a chronic condition like CHF can have psychological effects, including anxiety and depression. It is essential for individuals to:
Seek Psychological Support: Counseling or therapy can help individuals cope with the emotional aspects of living with a chronic illness.
Connect with Support Groups: Joining support groups for individuals with heart conditions can provide a sense of community and shared experiences.
Conclusion
Congestive heart failure is a serious condition that can significantly impact an individual’s life expectancy and quality of life. While the prognosis can vary widely based on several factors, including the stage of the disease and response to treatment, many individuals with CHF can manage their symptoms effectively and lead fulfilling lives.
Understanding the nature of CHF, adhering to treatment plans, and making lifestyle modifications are critical components of managing the condition. With proper care, support, and ongoing medical management, individuals with CHF can not only improve their life expectancy but also enhance their overall quality of life.
As research continues to advance in the field of cardiology, new treatments and management strategies will emerge, offering hope for improved outcomes for individuals living with congestive heart failure. By taking an active role in their health and seeking support, many patients can navigate the challenges of CHF and continue to enjoy meaningful and productive lives.
Related Topics: