An Implantable Cardioverter Defibrillator (ICD) is a life-saving device designed to treat dangerous arrhythmias (irregular heartbeats) and prevent sudden cardiac death (SCD) in individuals at high risk for life-threatening heart rhythm problems.
For those with heart conditions that cause abnormal rhythms, such as ventricular tachycardia or ventricular fibrillation, an ICD can be a crucial intervention that significantly reduces the risk of death. This article provides a comprehensive guide to ICDs, explaining how they work, their benefits, potential risks, and who might need one.
What Is An ICD?
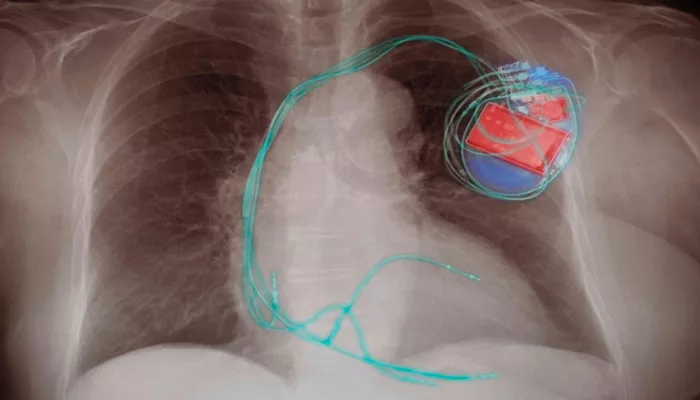
An Implantable Cardioverter Defibrillator (ICD) is a small electronic device that is surgically placed under the skin, typically in the chest area, to monitor and regulate the heart’s rhythm. The primary purpose of an ICD is to detect dangerous arrhythmias, such as ventricular fibrillation and ventricular tachycardia, and deliver a shock to restore a normal rhythm.
ICDs are similar in appearance and size to a pacemaker, but they have the added function of delivering high-energy shocks to the heart to stop abnormal rhythms. This action is essential in preventing sudden cardiac arrest (SCA), which can be fatal if not treated immediately.
Types of ICDs
There are several types of ICDs, each designed to meet the needs of patients with specific conditions. The main differences lie in the way the device functions and the complexity of its monitoring and pacing capabilities.
1. Single-Chamber ICD
A single-chamber ICD has one lead placed in either the right atrium or right ventricle of the heart. This type of ICD is generally used for individuals who only need monitoring of one chamber of the heart, typically the ventricles.
2. Dual-Chamber ICD
A dual-chamber ICD has two leads: one in the right atrium and one in the right ventricle. This type of ICD is more advanced, as it allows the device to monitor and regulate both the upper and lower chambers of the heart. It’s often used for people who have more complex arrhythmias or require dual-chamber pacing.
3. Biventricular ICD (Cardiac Resynchronization Therapy – CRT-D)
A biventricular ICD, also known as a Cardiac Resynchronization Therapy-Defibrillator (CRT-D), is designed for patients with heart failure and abnormal heart rhythms. This device has three leads: one in the right atrium, one in the right ventricle, and one in the left ventricle. CRT-D helps improve the coordination of heartbeats by resynchronizing the contractions of the heart’s ventricles, improving heart function and reducing arrhythmia risks.
How Do ICDs Work?
ICDs continuously monitor the heart’s electrical activity through electrodes placed inside the heart. If the device detects a dangerously fast or erratic heart rhythm, it will respond by sending an electrical shock to restore a normal rhythm. The shock is typically delivered through a wire (lead) that is connected to the heart.
There are several ways an ICD can treat arrhythmias:
1. Anti-Tachycardia Pacing (ATP)
In some cases, when the ICD detects a fast but regular rhythm (like ventricular tachycardia), it may use pacing to try to slow down the heart rate before a shock is needed. This treatment involves delivering small electrical pulses to the heart, which can sometimes break the abnormal rhythm and restore normal function.
2. Cardioversion
If ATP does not work, the ICD may deliver a synchronized shock to the heart to reset the rhythm. Cardioversion is typically used for less severe arrhythmias, and the shock is usually less intense than a defibrillation shock.
3. Defibrillation
In cases of life-threatening arrhythmias, such as ventricular fibrillation, the ICD delivers a stronger shock to the heart. This defibrillation shock is intended to stop the chaotic electrical activity and allow the heart to resume its normal rhythm.
4. Bradycardia Pacing
In addition to treating fast heart rhythms, some ICDs also have the ability to act as pacemakers. If the heart rate becomes too slow (bradycardia), the ICD will deliver pacing signals to the heart to ensure it beats at an adequate rate.
Why Do People Need ICDs?
ICDs are typically recommended for individuals at high risk for sudden cardiac arrest due to certain heart conditions or arrhythmias. These individuals may have experienced a life-threatening arrhythmia in the past or have certain conditions that increase their risk.
Here are some common reasons why people might need an ICD:
1. History of Sudden Cardiac Arrest
If a person has survived a sudden cardiac arrest episode, their doctor may recommend an ICD to prevent future incidents.
After experiencing a life-threatening arrhythmia, the risk of recurrence is significant, and an ICD can offer peace of mind by automatically monitoring and treating the condition.
2. Ventricular Arrhythmias
Ventricular tachycardia (VT) and ventricular fibrillation (VF) are life-threatening arrhythmias that originate in the lower chambers (ventricles) of the heart. These arrhythmias can cause the heart to stop pumping blood effectively, leading to sudden cardiac arrest. People with a history of VT or VF are often candidates for ICD implantation.
3. Heart Failure with Reduced Ejection Fraction
Individuals with heart failure and a reduced ejection fraction (HFrEF) are at higher risk of developing dangerous arrhythmias. When the heart’s pumping ability is weakened, it can trigger abnormal heart rhythms. An ICD can reduce the risk of sudden cardiac death in patients with this condition.
4. Inherited Heart Conditions
Some inherited heart conditions, such as Long QT Syndrome, Brugada Syndrome, or arrhythmogenic right ventricular dysplasia (ARVD), can increase the risk of life-threatening arrhythmias. Patients with these conditions may be advised to have an ICD to prevent sudden cardiac arrest.
5. Post-Myocardial Infarction (Heart Attack)
People who have had a heart attack are at an increased risk for arrhythmias, particularly if they have significant damage to the heart muscle. In such cases, an ICD may be implanted to prevent sudden cardiac arrest, particularly in individuals who are at a high risk of developing arrhythmias after a heart attack.
Benefits of ICDs
ICDs can provide numerous benefits to individuals with arrhythmias or heart conditions that put them at risk for sudden cardiac arrest. These include:
1. Prevention of Sudden Cardiac Death
The primary benefit of an ICD is its ability to prevent sudden cardiac death by delivering timely shocks to restore normal heart rhythm. In cases where a person is experiencing a life-threatening arrhythmia, the ICD can effectively intervene before it becomes fatal.
2. Improved Quality of Life
For individuals who are at risk of sudden cardiac death or frequent arrhythmias, having an ICD implanted can provide peace of mind. The knowledge that the device is constantly monitoring the heart can help reduce anxiety and improve quality of life.
3. Reduced Need for Hospitalization
ICDs can reduce the need for frequent hospital visits and emergency interventions. When the device detects an arrhythmia, it can deliver treatment immediately, potentially avoiding hospital stays for arrhythmia management or emergency care.
4. Life-saving Intervention
ICDs can provide a life-saving intervention for individuals who may otherwise not survive a sudden cardiac arrest. The shock delivered by the device can restore normal rhythm and prevent irreversible damage to the heart.
Risks And Side Effects of ICDs
While ICDs are generally safe and effective, they do come with some risks and potential side effects:
1. Infection
As with any surgery, there is a risk of infection when the ICD is implanted. Infections at the implantation site or in the heart’s leads can lead to serious complications, which may require further treatment or device removal.
2. Device Malfunction
Although rare, there is the possibility of a malfunction in the ICD. This can result in inappropriate shocks or a failure to deliver a shock when needed. Regular follow-up appointments are essential to ensure the device is functioning properly.
3. Psychological Impact
Some patients may experience anxiety or stress after having an ICD implanted, particularly if they experience a shock from the device. In some cases, this can affect their overall mental well-being.
4. Discomfort or Pain
After the device is implanted, some patients may experience discomfort or pain at the incision site. The leads may also cause irritation in some individuals, though this generally resolves over time.
Conclusion
An Implantable Cardioverter Defibrillator (ICD) is a vital device that can prevent sudden cardiac arrest and significantly improve the quality of life for individuals at high risk of life-threatening arrhythmias. By monitoring and correcting dangerous heart rhythms, an ICD can save lives and provide patients with peace of mind. However, as with any medical procedure, the decision to implant an ICD should be made with careful consideration of the patient’s health, risks, and overall condition.
Related topics: