Thromboembolism is a serious and potentially life-threatening condition in which a blood clot (thrombus) that forms in one part of the body breaks loose and travels through the bloodstream to another part of the body, causing a blockage (embolism). This blockage can occur in critical areas such as the lungs, brain, heart, or legs, leading to various complications. Depending on the location and severity of the embolism, thromboembolism can cause significant damage to vital organs, making early detection and treatment crucial.
In this article, we will explore the symptoms, causes, and treatment options for thromboembolism, providing a comprehensive overview of the condition to enhance understanding and awareness.
What is Thromboembolism?
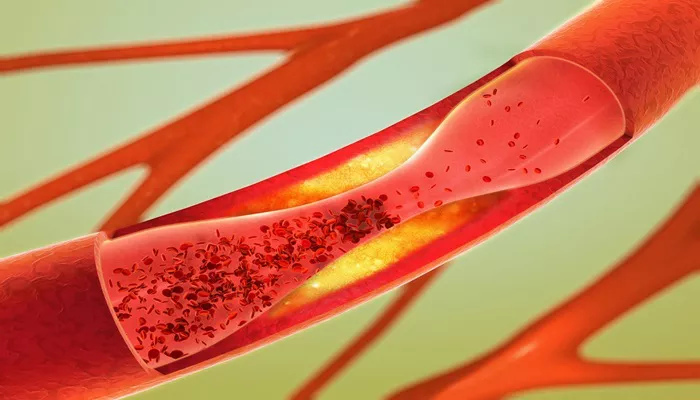
Thromboembolism is a condition that encompasses both the formation of blood clots (thrombosis) and the movement of these clots to distant sites in the body (embolism). A thrombus forms when blood coagulates abnormally, creating a clot that can obstruct normal blood flow. If this clot breaks off and travels through the bloodstream, it can block blood vessels in other parts of the body, leading to an embolism.
Thromboembolism can occur in various forms, including:
Pulmonary Embolism (PE): A clot that travels to the lungs, blocking the pulmonary artery or its branches.
Deep Vein Thrombosis (DVT): A clot that forms in the deep veins of the legs and can travel to the lungs.
Cerebral Embolism: A clot that blocks blood flow to the brain, potentially causing a stroke.
Coronary Embolism: A clot that blocks a coronary artery, leading to a heart attack.
The risk of thromboembolism can be influenced by a variety of factors, and understanding the symptoms and causes is crucial for early detection and prevention.
Causes of Thromboembolism
Thromboembolism can be caused by a range of factors that contribute to the formation of blood clots and increase the risk of their dislodging and traveling to other parts of the body. The most common causes and risk factors include:
1. Prolonged Immobility
One of the most common causes of thromboembolism is prolonged immobility, which can result from long periods of sitting, bed rest, or lack of physical activity. For instance, long flights, surgeries, or hospital stays often lead to reduced blood flow in the veins, increasing the risk of clot formation, especially in the lower legs (deep vein thrombosis).
2. Medical Conditions
Several medical conditions increase the risk of developing thromboembolism, including:
Atrial Fibrillation: This irregular heart rhythm can lead to the formation of clots in the heart, which may travel to the brain, causing a stroke.
Heart Disease: Conditions like heart failure and coronary artery disease can also contribute to the development of blood clots.
Cancer: Certain cancers, especially those affecting the pancreas, lungs, and ovaries, increase the risk of clot formation due to the secretion of clotting factors by cancer cells.
Obesity: Excess weight can put pressure on blood vessels, leading to poor circulation and an increased risk of clot formation.
Pregnancy: Pregnancy causes hormonal changes that increase the clotting tendency of the blood, which can elevate the risk of thromboembolism.
3. Genetic Factors
Some people have genetic conditions that predispose them to blood clots. These conditions are often referred to as “hypercoagulable states” and can increase the likelihood of developing thromboembolism. Examples include:
Factor V Leiden Mutation: A genetic mutation that makes the blood more likely to clot.
Prothrombin Gene Mutation: A genetic mutation that increases the level of prothrombin, a clotting factor in the blood.
4. Medications
Certain medications, such as oral contraceptives and hormone replacement therapy, can increase the risk of blood clot formation. These medications influence the levels of clotting factors in the blood, making it easier for clots to form.
5. Injury or Surgery
Injuries or surgeries that involve the blood vessels can lead to blood clot formation. After surgery, particularly orthopedic or abdominal surgery, there is a higher risk of developing deep vein thrombosis (DVT), which can result in thromboembolism.
6. Age
As people age, their blood vessels become less flexible, and the blood tends to flow more slowly. These changes increase the likelihood of blood clot formation, especially in older adults.
7. Smoking
Smoking damages blood vessels and disrupts normal circulation, which can increase the likelihood of clot formation.
Smokers are at higher risk of both DVT and pulmonary embolism.
Symptoms of Thromboembolism
The symptoms of thromboembolism vary depending on the location of the clot and the severity of the embolism. Recognizing the signs early can help with prompt medical intervention and prevent serious complications.
1. Pulmonary Embolism (PE)
Pulmonary embolism occurs when a blood clot blocks one or more arteries in the lungs. This is a life-threatening condition that requires immediate medical attention. Common symptoms include:
- Sudden shortness of breath
- Chest pain, especially when breathing deeply or coughing
- Coughing up blood (hemoptysis)
- Rapid heart rate (tachycardia)
- Dizziness or fainting
- Low blood oxygen levels
2. Deep Vein Thrombosis (DVT)
DVT occurs when a blood clot forms in the deep veins, usually in the legs. If left untreated, the clot can break loose and travel to the lungs, causing a pulmonary embolism. Common symptoms of DVT include:
- Swelling in one leg
- Pain or tenderness in the affected leg
- Red or discolored skin
- Warmth in the affected area
3. Cerebral Embolism (Stroke)
A cerebral embolism occurs when a clot travels to the brain and blocks blood flow to certain areas. This can lead to a stroke, which is a medical emergency. Symptoms of a stroke include:
Sudden numbness or weakness, especially on one side of the body.
Sudden confusion, trouble speaking, or difficulty understanding speech.
Sudden trouble seeing in one or both eyes.
Sudden trouble walking, dizziness, or loss of balance.
4. Coronary Embolism (Heart Attack)
A coronary embolism occurs when a clot blocks blood flow to the heart muscle, leading to a heart attack. Symptoms of a heart attack include:
- Chest pain or discomfort, often described as a heavy pressure or tightness
- Pain radiating to the arm, jaw, neck, or back
- Shortness of breath
- Sweating
- Nausea or vomiting
Treatment for Thromboembolism
The treatment of thromboembolism depends on the type, severity, and location of the embolism. The primary goal of treatment is to prevent the clot from causing further damage and to reduce the risk of future clots. Treatment options include:
1. Anticoagulants (Blood Thinners)
The most common treatment for thromboembolism involves the use of anticoagulants, also known as blood thinners. These medications work by preventing further clot formation and allowing the body to dissolve the existing clot. Common anticoagulants include:
Heparin: A fast-acting anticoagulant often administered intravenously in hospitals.
Warfarin: An oral anticoagulant used for long-term prevention of clots.
Direct Oral Anticoagulants (DOACs): These newer anticoagulants, such as rivaroxaban and apixaban, are increasingly used due to their effectiveness and lower risk of bleeding complications.
2. Thrombolytic Therapy
In cases where the clot is life-threatening or causing significant damage, thrombolytic therapy may be used. These medications, also known as clot-busters, are designed to dissolve the clot quickly.
Thrombolytic therapy is often used in emergency situations, such as with pulmonary embolism or stroke.
3. Surgical Intervention
In some cases, surgical intervention may be required to remove the clot. This is typically done in severe cases of thromboembolism where other treatments have not been effective. Surgical options include:
Embolectomy: Surgical removal of the clot.
Inferior Vena Cava (IVC) Filter: A device implanted in the vena cava to catch and prevent blood clots from traveling to the lungs.
4. Compression Stockings
For individuals with DVT, wearing compression stockings can help reduce swelling and improve blood flow in the legs, decreasing the risk of further clot formation.
Prevention of Thromboembolism
Preventing thromboembolism involves managing risk factors and taking steps to improve circulation. Key preventive measures include:
- Staying active and avoiding prolonged immobility
- Maintaining a healthy weight
- Quitting smoking
- Managing underlying conditions such as diabetes, hypertension, and high cholesterol
- Using blood thinners as prescribed by a doctor for those at high risk
Conclusion
Thromboembolism is a serious condition that can have significant consequences for health and well-being. Early detection, prompt treatment, and preventive measures are key to managing the risk of thromboembolism and reducing the risk of complications. Understanding the symptoms, causes, and treatment options for thromboembolism is essential for both patients and healthcare providers to ensure optimal care and outcomes.
Related topics: