Left ventricular systolic dysfunction (LVSD) is a condition in which the left ventricle of the heart is unable to contract effectively and pump blood to the rest of the body. This dysfunction is one of the most common causes of heart failure and can lead to significant symptoms, complications, and a decreased quality of life if not properly managed. Understanding LVSD is crucial for early diagnosis and treatment, as it can help prevent progression to more severe heart conditions.
In this article, we will explore the causes, symptoms, and treatment options for Left Ventricular Systolic Dysfunction, providing a comprehensive understanding of the condition and its management.
What Is Left Ventricular Systolic Dysfunction (LVSD)?
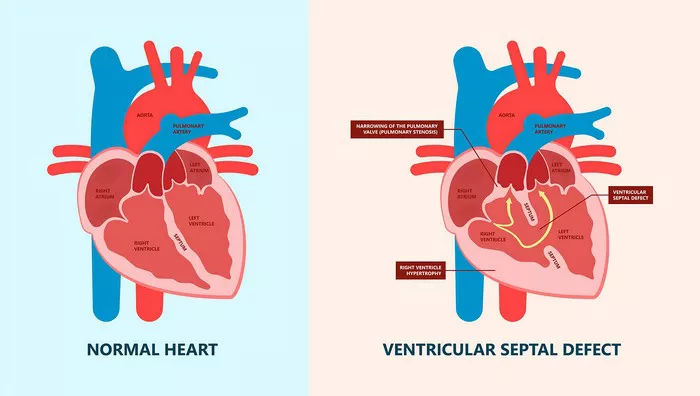
The heart consists of four chambers: two atria and two ventricles. The left ventricle is responsible for pumping oxygen-rich blood to the entire body, except the lungs. When the left ventricle fails to contract properly, the heart’s ability to pump blood is compromised. This leads to insufficient blood supply to vital organs and tissues, resulting in symptoms such as shortness of breath, fatigue, and swelling in the legs and ankles.
LVSD occurs when the left ventricle’s ejection fraction (EF) is reduced. Ejection fraction is the percentage of blood pumped out of the left ventricle with each heartbeat. A normal EF is typically between 50% and 70%. When EF falls below 40%, it is considered to indicate systolic dysfunction, and the heart’s ability to efficiently pump blood is compromised.
Causes of Left Ventricular Systolic Dysfunction (LVSD)
The causes of LVSD can vary, and the condition may arise due to several underlying factors. These causes include:
1. Coronary Artery Disease (CAD)
Coronary artery disease is the leading cause of LVSD. It occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked due to the buildup of fatty deposits (plaque). This blockage reduces blood flow to the heart, causing ischemia (lack of oxygen), which can weaken the heart muscle and impair its ability to contract effectively.
2. Myocardial Infarction (Heart Attack)
A heart attack occurs when a coronary artery is completely blocked, leading to a loss of blood flow to part of the heart muscle. The affected part of the heart muscle may become damaged or die, resulting in reduced contractility of the left ventricle. Post-heart attack, the heart tissue may heal with scar tissue, which further impairs the heart’s ability to pump blood.
3. Hypertension (High Blood Pressure)
Chronic high blood pressure forces the heart to work harder to pump blood, which can lead to left ventricular hypertrophy (enlargement of the left ventricle). Over time, the heart muscle may become stiff and less able to contract effectively, leading to systolic dysfunction. Hypertension is one of the most common risk factors for LVSD.
4. Dilated Cardiomyopathy
Dilated cardiomyopathy (DCM) is a condition in which the heart’s chambers, particularly the left ventricle, become enlarged and weakened. The heart’s ability to contract and pump blood effectively is reduced. DCM can be caused by a variety of factors, including genetic predisposition, viral infections, alcohol abuse, and certain medications or chemotherapy treatments.
5. Valvular Heart Disease
Conditions affecting the heart valves, such as mitral regurgitation or aortic stenosis, can lead to LVSD. These valve abnormalities can increase the workload on the left ventricle, eventually leading to its dysfunction. In mitral regurgitation, for instance, the mitral valve does not close properly, causing blood to flow backward into the left atrium, which increases the pressure in the left ventricle and ultimately damages its function.
6. Arrhythmias
Certain arrhythmias, especially persistent atrial fibrillation or ventricular arrhythmias, can impair the left ventricle’s ability to contract properly. Prolonged arrhythmias can lead to abnormal electrical signaling in the heart, weakening the heart muscle and contributing to systolic dysfunction.
7. Infections and Inflammatory Diseases
Infections such as myocarditis (inflammation of the heart muscle) can damage the left ventricle and lead to LVSD. Inflammatory diseases like lupus or rheumatoid arthritis can also cause inflammation of the heart muscle, which can reduce the heart’s pumping ability.
8. Toxins and Medications
Chronic alcohol abuse, certain chemotherapy drugs, and illicit drugs such as cocaine can damage the heart muscle and lead to LVSD. In these cases, the heart muscle is weakened or destroyed, impairing its ability to contract and pump blood effectively.
9. Genetics
In some cases, LVSD may be caused by inherited genetic conditions such as familial dilated cardiomyopathy. Individuals with a family history of heart failure or heart muscle disease may be at higher risk of developing LVSD.
Symptoms of Left Ventricular Systolic Dysfunction (LVSD)
The symptoms of LVSD are often related to the heart’s inability to pump blood effectively, leading to reduced oxygen and nutrient delivery to tissues and organs. The severity of symptoms may depend on the extent of the dysfunction and its underlying cause.
1. Fatigue
One of the most common symptoms of LVSD is fatigue, as the body’s organs and tissues do not receive adequate blood flow.
As a result, individuals may experience a general lack of energy, making even simple tasks exhausting.
2. Shortness of Breath (Dyspnea)
As the left ventricle fails to pump blood efficiently, fluid can accumulate in the lungs, causing shortness of breath. This symptom is often more noticeable during physical exertion or when lying flat (orthopnea). In severe cases, it may also occur at rest.
3. Swelling (Edema)
Reduced blood flow and fluid retention are common in LVSD. Swelling may develop in the feet, ankles, legs, or abdomen.
This occurs because the heart’s inability to pump blood efficiently causes fluid to accumulate in the body.
4. Palpitations
Individuals with LVSD may experience irregular heart rhythms or palpitations, particularly when the heart is under stress or working harder to compensate for the reduced pumping ability.
5. Cough
A persistent cough, often worse when lying down, is a common symptom of LVSD due to fluid buildup in the lungs. This condition is called pulmonary congestion and can lead to a dry, hacking cough or even wheezing.
6. Decreased Exercise Tolerance
People with LVSD may notice a significant reduction in their ability to exercise or perform physical activities. This is due to insufficient oxygen delivery to the muscles and other organs, leading to fatigue and weakness during activity.
7. Dizziness and Lightheadedness
As the heart struggles to pump blood, blood pressure may drop, leading to dizziness, lightheadedness, or fainting, especially when standing up quickly.
8. Weight Gain
Sudden or unexplained weight gain may occur due to fluid retention, which is a common symptom of LVSD. The buildup of fluid in the body can lead to noticeable increases in weight, especially in the abdomen or lower extremities.
Treatment for Left Ventricular Systolic Dysfunction (LVSD)
The treatment of LVSD primarily focuses on improving heart function, relieving symptoms, and preventing complications.
The approach to treatment depends on the underlying cause of the dysfunction, the severity of the condition, and the presence of other health problems. Treatment may involve lifestyle changes, medications, and in some cases, surgical interventions.
1. Lifestyle Modifications
Making lifestyle changes is a critical part of managing LVSD and improving heart health. Some essential lifestyle modifications include:
Diet: A heart-healthy diet low in salt, saturated fats, and cholesterol can help reduce the workload on the heart. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins is recommended.
Exercise: Regular physical activity, as recommended by a healthcare provider, can strengthen the heart and improve overall cardiovascular health. However, intense exercise should be avoided if symptoms are severe.
Smoking Cessation: Quitting smoking is crucial for managing LVSD, as smoking accelerates the progression of heart disease and increases the risk of complications.
Weight Management: Maintaining a healthy weight can reduce the strain on the heart and improve overall cardiovascular function.
2. Medications
Several medications can be prescribed to manage LVSD and improve heart function:
Angiotensin-Converting Enzyme (ACE) Inhibitors: These medications help relax blood vessels, reduce blood pressure, and improve blood flow to the heart.
Beta-Blockers: Beta-blockers help reduce heart rate and blood pressure, decreasing the heart’s workload and improving its pumping ability.
Diuretics: Diuretics help reduce fluid buildup in the body, relieving symptoms such as swelling and shortness of breath.
Aldosterone Antagonists: Medications like spironolactone help block the effects of aldosterone, a hormone that can increase fluid retention and worsen heart failure.
Angiotensin II Receptor Blockers (ARBs): These medications work similarly to ACE inhibitors by relaxing blood vessels and lowering blood pressure.
Inotropes: Inotropes, such as digoxin, can help improve the contractility of the heart muscle, making it pump more effectively.
3. Implantable Devices
In severe cases of LVSD, medical devices may be implanted to help the heart pump blood more effectively:
Implantable Cardioverter-Defibrillators (ICDs): An ICD is used to monitor and correct abnormal heart rhythms, preventing life-threatening arrhythmias in patients with LVSD.
Cardiac Resynchronization Therapy (CRT): CRT involves implanting a pacemaker-like device that helps synchronize the contractions of the heart’s chambers, improving the heart’s ability to pump blood.
4. Surgical Interventions
In some cases, surgical interventions may be necessary to treat the underlying causes of LVSD or to repair damage:
Coronary Artery Bypass Surgery (CABG): If LVSD is caused by coronary artery disease, bypass surgery may be performed to restore blood flow to the heart muscle.
Heart Valve Surgery: If a valve disorder is contributing to LVSD, valve repair or replacement may be recommended.
Heart Transplant: In severe cases where LVSD has progressed to end-stage heart failure, a heart transplant may be considered for patients who are otherwise healthy enough to undergo surgery.
Conclusion
Left Ventricular Systolic Dysfunction (LVSD) is a serious condition that affects the heart’s ability to pump blood efficiently, leading to a range of symptoms and complications. Early detection, appropriate treatment, and lifestyle modifications are essential for managing LVSD and preventing progression to more severe heart failure. If you are at risk of LVSD or experiencing symptoms, consult a healthcare provider for a thorough evaluation and personalized treatment plan.
Related topics: