Osteoarthritis (OA) is the most common form of arthritis, characterized by the degeneration of cartilage and the underlying bone in joints. It leads to pain, stiffness, and decreased mobility, significantly impacting the quality of life. While aging and mechanical stress are well-known contributors to OA, emerging evidence suggests that various metabolic diseases can also play a significant role in the development and progression of osteoarthritis. This article explores the metabolic diseases associated with osteoarthritis, their mechanisms, implications for joint health, and management strategies.
Understanding Osteoarthritis
What is Osteoarthritis?
Osteoarthritis is a degenerative joint disease that primarily affects the cartilage—the smooth, protective tissue that cushions the ends of bones in joints. As the cartilage wears away, bones may rub against each other, leading to pain, swelling, and loss of joint function. OA can affect any joint in the body but commonly impacts weight-bearing joints such as the knees, hips, and spine.
Symptoms of Osteoarthritis
The symptoms of osteoarthritis can vary in severity and may include:
- Joint pain and tenderness
- Stiffness, especially after periods of inactivity
- Swelling around the joint
- Reduced range of motion
- A grating sensation or popping sound during movement
Risk Factors for Osteoarthritis
Several risk factors contribute to the development of osteoarthritis, including:
Age: The risk of OA increases with age.
Obesity: Excess weight places additional stress on weight-bearing joints.
Joint injuries: Previous injuries can increase the risk of OA.
Genetics: A family history of OA may predispose individuals to the condition.
Gender: Women are more likely to develop OA, especially after menopause.
Metabolic Diseases Associated with Osteoarthritis
Several metabolic diseases have been linked to the development and progression of osteoarthritis. Understanding these conditions can provide insight into the multifactorial nature of OA.
Obesity
Obesity is a complex metabolic disease characterized by excessive fat accumulation that poses health risks. It is a significant risk factor for osteoarthritis, particularly in weight-bearing joints.
Mechanism
The relationship between obesity and osteoarthritis is multifaceted:
Mechanical Stress: Excess body weight increases the load on weight-bearing joints, leading to accelerated cartilage wear and tear.
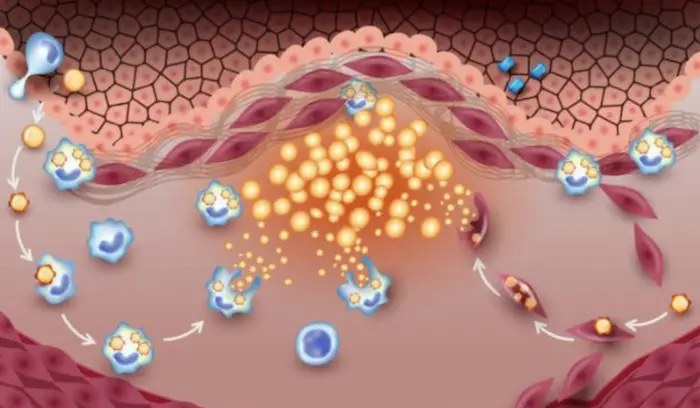
Inflammation: Adipose tissue (fat) produces pro-inflammatory cytokines, which can contribute to joint inflammation and degradation of cartilage.
Metabolic Changes: Obesity is associated with insulin resistance and metabolic syndrome, which can further exacerbate joint health.
Management
Weight loss through diet and exercise can significantly reduce the risk of developing OA and alleviate symptoms in those already affected. A balanced diet rich in anti-inflammatory foods and regular physical activity are key components of management.
Diabetes Mellitus
Diabetes mellitus, particularly type 2 diabetes, is a chronic metabolic disorder characterized by high blood sugar levels due to insulin resistance or insufficient insulin production. Diabetes has been linked to an increased risk of osteoarthritis.
Mechanism
The connection between diabetes and osteoarthritis may involve:
Advanced Glycation End Products (AGEs): High blood sugar levels lead to the formation of AGEs, which can accumulate in joint tissues and contribute to inflammation and cartilage degradation.
Inflammation: Diabetes is associated with chronic low-grade inflammation, which can exacerbate joint damage.
Neuropathy: Diabetic neuropathy can lead to altered biomechanics and joint loading, increasing the risk of OA.
Management
Managing diabetes through blood sugar control, weight management, and a healthy lifestyle can help reduce the risk of osteoarthritis. Regular monitoring and intervention are essential for preventing complications.
Metabolic Syndrome
Metabolic syndrome is a cluster of conditions—including obesity, hypertension, high blood sugar, and dyslipidemia—that increase the risk of cardiovascular disease and diabetes. It is also associated with an increased risk of osteoarthritis.
Mechanism
The components of metabolic syndrome can contribute to osteoarthritis through:
Chronic Inflammation: The presence of multiple metabolic abnormalities can lead to increased inflammation, negatively impacting joint health.
Altered Lipid Metabolism: Dyslipidemia can influence joint tissue metabolism and contribute to cartilage degradation.
Insulin Resistance: Insulin resistance can promote inflammatory pathways that damage joint tissues.
Management
Addressing metabolic syndrome involves lifestyle modifications, including weight loss, regular physical activity, and dietary changes. Managing individual components, such as hypertension and dyslipidemia, is also crucial.
Hyperuricemia and Gout
Hyperuricemia is a condition characterized by elevated levels of uric acid in the blood, which can lead to gout—a type of inflammatory arthritis. While gout is distinct from osteoarthritis, the two conditions can coexist.
Mechanism
The relationship between hyperuricemia and osteoarthritis may involve:
Inflammation: Gout attacks can lead to joint inflammation, which may exacerbate underlying osteoarthritis.
Crystal Deposition: Uric acid crystals can deposit in joints, causing pain and inflammation, contributing to joint damage over time.
Management
Management of hyperuricemia involves lifestyle changes, dietary modifications, and medications to lower uric acid levels. Addressing gout flares promptly can help prevent further joint damage.
Osteoporosis
Osteoporosis is a metabolic bone disease characterized by decreased bone density and increased fracture risk. While primarily affecting bones, osteoporosis can also impact joint health and contribute to osteoarthritis.
Mechanism
The relationship between osteoporosis and osteoarthritis may involve:
Joint Stability: Decreased bone density can lead to joint instability, increasing the risk of joint degeneration and OA.
Inflammation: Osteoporosis is associated with inflammatory processes that can affect cartilage health.
Management
Managing osteoporosis involves lifestyle changes, including weight-bearing exercises, adequate calcium and vitamin D intake, and medications to improve bone density. Maintaining joint health through these interventions can help prevent or mitigate OA.
Thyroid Disorders
Thyroid disorders, including hypothyroidism and hyperthyroidism, can impact various metabolic processes in the body. Both conditions have been linked to osteoarthritis.
Mechanism
The relationship between thyroid disorders and osteoarthritis may include:
Metabolic Changes: Thyroid hormones play a crucial role in bone and cartilage metabolism. Imbalances can lead to joint degradation.
Inflammation: Autoimmune thyroid disorders can contribute to systemic inflammation, negatively impacting joint health.
Management
Managing thyroid disorders through appropriate hormonal treatment can help mitigate their impact on joint health. Regular monitoring and adjustments may be necessary to maintain optimal thyroid function.
Vitamin D Deficiency
Vitamin D is essential for bone health and plays a role in cartilage metabolism. Deficiency in vitamin D has been associated with an increased risk of osteoarthritis.
Mechanism
The connection between vitamin D deficiency and osteoarthritis may involve:
Bone Health: Vitamin D is crucial for calcium absorption and bone density. Deficiency can weaken bones and affect joint stability.
Inflammation: Vitamin D has anti-inflammatory properties, and its deficiency may contribute to increased inflammation in joints.
Management
Ensuring adequate vitamin D levels through sunlight exposure, diet, and supplementation can help support bone and joint health. Regular monitoring of vitamin D levels is essential, especially in at-risk populations.
Other Metabolic Disorders
Other metabolic disorders, such as certain lipid metabolism disorders and mitochondrial diseases, may also contribute to osteoarthritis through various mechanisms, including inflammation, altered joint mechanics, and metabolic dysregulation.
Implications of Metabolic Diseases on Osteoarthritis
Quality of Life
The presence of metabolic diseases can significantly impact the quality of life for individuals with osteoarthritis. Chronic pain, reduced mobility, and the inability to perform daily activities can lead to physical and emotional distress.
Nutritional Considerations
Diet plays a crucial role in managing both metabolic diseases and osteoarthritis. A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and healthy fats, can help reduce inflammation and support joint health. Specific dietary interventions may be necessary based on individual metabolic conditions.
Monitoring and Management
For individuals with metabolic diseases and osteoarthritis, regular monitoring and comprehensive management are essential. This may include:
Regular Check-ups: Routine evaluations to monitor joint health and metabolic conditions.
Physical Therapy: Tailored exercise programs to improve joint function and reduce pain.
Medications: Appropriate medications to manage pain, inflammation, and underlying metabolic conditions.
Conclusion
Osteoarthritis is a multifaceted condition influenced by various factors, including metabolic diseases such as obesity, diabetes, metabolic syndrome, hyperuricemia, osteoporosis, thyroid disorders, and vitamin D deficiency. Understanding the connections between these metabolic conditions and osteoarthritis can inform prevention and management strategies. By addressing the underlying metabolic issues, individuals can improve their joint health, reduce symptoms, and enhance their overall quality of life. If you suspect you are at risk for osteoarthritis or have metabolic concerns, it is essential to consult with healthcare professionals for proper evaluation and tailored management plans.
Related Topics: