Metabolic diseases, encompassing a range of conditions such as obesity, type 2 diabetes, metabolic syndrome, and dyslipidemia, have become increasingly prevalent in modern society. These disorders are characterized by abnormalities in the body’s metabolic processes, leading to significant health complications, including cardiovascular disease, kidney dysfunction, and increased mortality risk. With the rising incidence of these conditions, a critical question arises: Can metabolic disease be cured? This article delves into the nature of metabolic diseases, their underlying mechanisms, current treatment strategies, and the potential for long-term remission or cure.
Understanding Metabolic Disease
Definition of Metabolic Disease
Metabolic diseases refer to a group of disorders that disrupt normal metabolic processes in the body. These disorders can affect how the body converts food into energy, how it stores fat, and how it processes nutrients, leading to various health issues. The most common metabolic diseases include:
Obesity: Excessive body fat accumulation that can impair health.
Type 2 Diabetes Mellitus: A condition characterized by insulin resistance and elevated blood sugar levels.
Metabolic Syndrome: A cluster of conditions, including hypertension, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels, that increase the risk of heart disease and stroke.
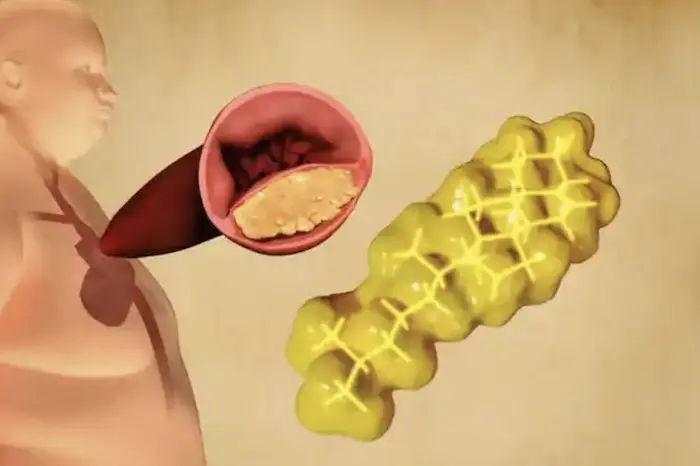
Dyslipidemia: Abnormal levels of lipids in the blood, including high levels of LDL cholesterol and triglycerides.
Causes of Metabolic Disease
The development of metabolic diseases is influenced by a combination of genetic, environmental, and lifestyle factors:
Genetics: Family history and genetic predisposition can increase the risk of developing metabolic diseases.
Lifestyle Factors: Poor dietary choices, physical inactivity, and sedentary behavior are significant contributors to the development of metabolic disorders.
Environmental Factors: Socioeconomic status, access to healthcare, and exposure to environmental toxins can impact metabolic health.
Mechanisms of Metabolic Disease Development
Insulin Resistance
Insulin resistance is a hallmark of many metabolic diseases, particularly type 2 diabetes and metabolic syndrome. It occurs when the body’s cells become less responsive to insulin, a hormone that regulates blood sugar levels. As a result, the pancreas produces more insulin to compensate, leading to elevated insulin levels (hyperinsulinemia) and eventually, pancreatic beta-cell dysfunction.
Inflammation
Chronic low-grade inflammation is often associated with obesity and metabolic diseases. Adipose (fat) tissue secretes pro-inflammatory cytokines, which can contribute to insulin resistance and other metabolic disturbances. This inflammatory response can also lead to endothelial dysfunction, increasing the risk of cardiovascular disease.
Mitochondrial Dysfunction
Mitochondria are the energy-producing organelles in cells, and their dysfunction can impair metabolic processes. Mitochondrial dysfunction is linked to obesity, insulin resistance, and other metabolic disorders, as it affects the body’s ability to oxidize fats and carbohydrates efficiently.
Gut Microbiota
The gut microbiome plays a crucial role in metabolism, and alterations in gut bacteria composition (dysbiosis) have been linked to metabolic diseases. Dysbiosis can influence energy extraction from food, inflammation, and insulin sensitivity.
Current Treatment Strategies for Metabolic Disease
Lifestyle Modifications
Dietary Changes: Adopting a balanced, nutritious diet is fundamental for managing metabolic diseases. Key dietary strategies include:
Whole Foods: Emphasizing whole, minimally processed foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats.
Portion Control: Being mindful of portion sizes to avoid overeating.
Low Glycemic Index Foods: Choosing foods with a low glycemic index to help stabilize blood sugar levels.
Reducing Added Sugars and Refined Carbohydrates: Limiting the intake of sugary beverages, sweets, and refined grains.
Physical Activity: Regular physical activity is essential for improving metabolic health. Recommendations include:
Aerobic Exercise: Engaging in at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, or swimming.
Strength Training: Incorporating resistance training exercises at least two days a week to build muscle mass and improve metabolism.
Incorporating Movement: Finding opportunities to be active throughout the day, such as taking the stairs, walking during breaks, or gardening.
Medical Interventions
Medications: For some individuals, medications may be necessary to manage blood sugar levels, cholesterol, or blood pressure. Common classes of medications include:
Metformin: Often prescribed for type 2 diabetes to improve insulin sensitivity and lower blood sugar levels.
GLP-1 Receptor Agonists: Medications that stimulate insulin secretion and promote weight loss.
SGLT2 Inhibitors: Drugs that help lower blood sugar levels by promoting glucose excretion in the urine.
Bariatric Surgery: For individuals with severe obesity, bariatric surgery can induce significant weight loss and improve metabolic health. Studies have shown that many patients experience remission of type 2 diabetes following surgery.
Emerging Therapies
Research is ongoing to explore new therapies for reversing metabolic diseases:
Metabolic Surgery: Beyond traditional bariatric surgery, newer techniques are being studied for their potential to improve metabolic health.
Pharmacotherapy: Investigational drugs targeting metabolic pathways are being developed to improve insulin sensitivity and promote weight loss.
Gene Therapy: Emerging research in gene therapy aims to modify genes associated with metabolic diseases, potentially offering new avenues for treatment.
The Question of Cure: Can Metabolic Disease Be Cured?
Evidence Supporting Reversal and Remission
Research indicates that many metabolic diseases can be reversed or significantly improved through lifestyle modifications and medical interventions. Here are some key findings:
Obesity: Weight loss through dietary changes and increased physical activity can lead to significant improvements in metabolic health. Studies have shown that even modest weight loss (5-10% of body weight) can lead to improvements in insulin sensitivity, blood pressure, and lipid levels.
Type 2 Diabetes: Lifestyle interventions, such as a low-calorie diet and regular physical activity, can lead to remission of type 2 diabetes. The Diabetes Prevention Program (DPP) demonstrated that participants who lost 5-7% of their body weight and engaged in regular exercise reduced their risk of developing diabetes by 58%.
Metabolic Syndrome: Addressing multiple components of metabolic syndrome through lifestyle changes can lead to significant improvements. A study published in the Journal of the American College of Cardiology found that participants who adopted a heart-healthy lifestyle experienced reductions in blood pressure, cholesterol levels, and waist circumference.
Dyslipidemia: Changes in diet, such as adopting a Mediterranean diet rich in healthy fats, fruits, and vegetables, can improve lipid profiles. Regular physical activity also contributes to better lipid management.
Limitations and Challenges
While there is evidence supporting the reversibility of metabolic diseases, several challenges can hinder progress:
Genetic Factors: Genetic predisposition can make it more difficult for some individuals to achieve and maintain metabolic health.
Behavioral Factors: Lifestyle changes require sustained motivation and commitment, and many individuals struggle with adherence to dietary and exercise recommendations.
Socioeconomic Barriers: Access to healthy food options, safe environments for physical activity, and healthcare resources can impact an individual’s ability to make necessary lifestyle changes.
Psychological Factors: Mental health conditions, such as depression and anxiety, can affect motivation and the ability to engage in healthy behaviors.
Strategies for Achieving Long-Term Remission
Comprehensive Lifestyle Changes
Achieving long-term remission from metabolic diseases often requires comprehensive lifestyle changes that address diet, physical activity, and behavioral modifications. Key strategies include:
Sustainable Diet: Focusing on a balanced diet that can be maintained long-term rather than short-term fad diets.
Regular Exercise: Establishing a consistent exercise routine that incorporates both aerobic and strength-training activities.
Behavioral Support: Seeking support from healthcare professionals, nutritionists, or support groups to stay motivated and accountable.
Regular Monitoring and Follow-Up
Ongoing monitoring of metabolic health is essential for individuals with a history of metabolic disease. Regular check-ups, blood tests, and assessments can help track progress and identify any potential issues early on.
Education and Awareness
Increasing awareness about metabolic diseases, their risk factors, and the importance of prevention is crucial. Educational programs and community initiatives can empower individuals to make informed decisions about their health.
Personalized Treatment Plans
Recognizing that each individual is unique, personalized treatment plans that consider genetic, behavioral, and environmental factors can enhance the effectiveness of interventions. Healthcare providers should work collaboratively with patients to develop tailored strategies for achieving and maintaining metabolic health.
Conclusion
The question of whether metabolic disease can be cured is complex and multifaceted. While there is substantial evidence that many metabolic conditions, including obesity, type 2 diabetes, and metabolic syndrome, can be reversed or significantly improved through lifestyle modifications and medical interventions, the journey toward remission is not without its challenges.
Genetic predisposition, behavioral factors, socioeconomic barriers, and psychological conditions can all impact an individual’s ability to achieve and maintain metabolic health. However, with commitment, support, and access to resources, many individuals can experience meaningful improvements in their metabolic health and reduce the risk of associated complications.
As research continues to evolve, the potential for new therapies and interventions to enhance metabolic health remains promising. By promoting awareness, education, and access to resources, we can empower individuals to take charge of their health and work towards reversing metabolic diseases. Ultimately, while a definitive cure may not yet be available for all metabolic diseases, significant progress can be made toward long-term remission and improved quality of life.
Related Topics: