Metabolic diseases are a group of disorders that disrupt normal metabolism, the process by which the body converts food into energy. These diseases can lead to various health issues, including obesity, type 2 diabetes, metabolic syndrome, and cardiovascular diseases. Understanding when metabolic diseases occur is crucial for prevention, early detection, and effective management. This article explores the factors contributing to the onset of metabolic diseases, their prevalence, and the role of lifestyle, genetics, and environmental influences.
Understanding Metabolic Diseases
Definition of Metabolic Diseases
Metabolic diseases refer to a range of conditions that affect how the body processes or utilizes nutrients. They can be categorized into several types, including:
Obesity: Characterized by excessive body fat accumulation, obesity is a significant risk factor for many metabolic diseases.
Type 2 Diabetes Mellitus: A chronic condition marked by insulin resistance and high blood glucose levels.
Metabolic Syndrome: A cluster of conditions, including hypertension, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels.
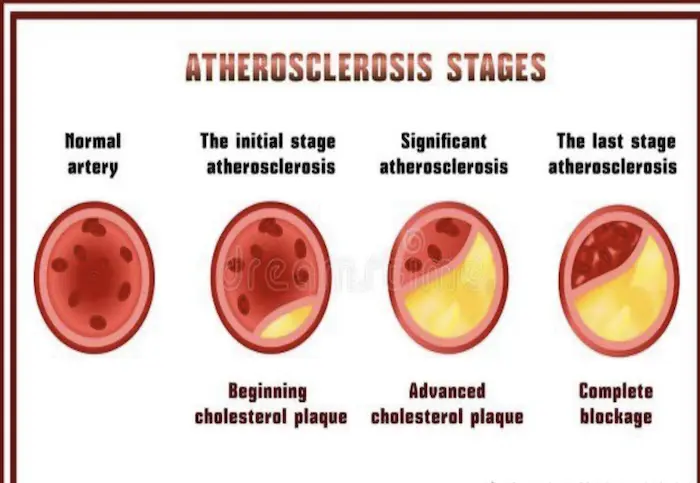
Dyslipidemia: Abnormal levels of lipids in the blood, which can increase the risk of cardiovascular diseases.
Causes of Metabolic Diseases
Metabolic diseases arise from a combination of genetic, environmental, and lifestyle factors. Understanding these causes is essential for identifying when these diseases may occur.
Factors Contributing to the Onset of Metabolic Diseases
Genetic Factors
Genetics play a significant role in the development of metabolic diseases. Certain genetic predispositions can increase an individual’s risk of developing conditions such as obesity and type 2 diabetes. Key points include:
Family History: A family history of metabolic diseases often indicates a higher likelihood of developing similar conditions. For example, if parents or siblings have type 2 diabetes, the risk for other family members increases.
Genetic Mutations: Specific genetic mutations can affect metabolism, leading to conditions such as familial hypercholesterolemia, which results in high cholesterol levels.
Age
Age is a critical factor in the development of metabolic diseases. As individuals age, their metabolism naturally slows down, and the risk of developing metabolic disorders increases. Key insights include:
Increased Insulin Resistance: Older adults often experience increased insulin resistance, making them more susceptible to type 2 diabetes.
Changes in Body Composition: Aging is associated with a decrease in muscle mass and an increase in body fat, particularly visceral fat, which is linked to metabolic diseases.
Lifestyle Factors
Lifestyle choices significantly impact metabolic health. Poor dietary habits, physical inactivity, and unhealthy behaviors contribute to the onset of metabolic diseases. Key lifestyle factors include:
Diet
High-Calorie Diets: Diets high in calories, particularly from processed foods, sugars, and unhealthy fats, can lead to weight gain and obesity, increasing the risk of metabolic diseases.
Low Nutrient Density: A diet lacking in essential nutrients can impair metabolic function and contribute to conditions like insulin resistance.
Physical Inactivity
Sedentary Lifestyle: A lack of physical activity is strongly associated with obesity and metabolic diseases. Regular exercise helps regulate weight, improve insulin sensitivity, and maintain cardiovascular health.
Impact of Modern Life: The rise of sedentary occupations and leisure activities, such as prolonged screen time, has contributed to decreased physical activity levels in many populations.
Smoking and Alcohol Consumption
Smoking: Tobacco use is linked to various metabolic disorders, including insulin resistance and increased abdominal fat.
Excessive Alcohol Intake: Heavy drinking can lead to weight gain, liver disease, and dyslipidemia, all of which increase the risk of metabolic diseases.
Environmental Influences
Environmental factors can also contribute to the development of metabolic diseases. These factors include:
Socioeconomic Status
Access to Healthy Foods: Individuals in lower socioeconomic groups may have limited access to healthy food options, leading to poor dietary choices and increased risk of obesity and metabolic diseases.
Healthcare Access: Limited access to healthcare services can hinder early detection and management of metabolic disorders.
Urbanization and Lifestyle Changes
Urban Environments: Rapid urbanization often leads to lifestyle changes that promote sedentary behavior and unhealthy eating habits.
Cultural Influences: Cultural attitudes toward diet, exercise, and health can influence the prevalence of metabolic diseases in different populations.
Psychological Factors
Mental health can significantly impact metabolic health. Conditions such as depression and anxiety can lead to unhealthy lifestyle choices, including poor eating habits and physical inactivity. Key points include:
Emotional Eating: Individuals dealing with stress or emotional issues may turn to food for comfort, leading to weight gain and increased risk of metabolic diseases.
Impact on Motivation: Mental health issues can reduce motivation to engage in physical activity and maintain a healthy diet.
When Do Metabolic Diseases Occur?
Childhood and Adolescence
Metabolic diseases can begin in childhood and adolescence, often influenced by lifestyle and dietary habits. Key trends include:
Childhood Obesity: The prevalence of obesity among children has increased dramatically in recent decades. Factors such as poor diet, lack of physical activity, and increased screen time contribute to this trend.
Early Onset of Type 2 Diabetes: There has been a concerning rise in type 2 diabetes cases among adolescents, often linked to obesity and sedentary lifestyles.
Young Adulthood
Young adulthood is another critical period for the development of metabolic diseases. Key points include:
Lifestyle Transitions: Transitioning to independent living, such as moving away from home for college or work, can lead to changes in diet and physical activity levels.
Increased Stress: Young adults may experience increased stress from work and personal responsibilities, leading to unhealthy coping mechanisms, such as poor eating habits and reduced physical activity.
Middle Age
Middle age is a significant period for the onset of metabolic diseases. Key insights include:
Weight Gain: Many individuals experience weight gain during middle age due to hormonal changes, decreased metabolism, and lifestyle factors.
Increased Risk of Chronic Conditions: The risk of developing conditions such as type 2 diabetes, hypertension, and dyslipidemia increases during this stage of life.
Older Adults
The risk of metabolic diseases continues to rise in older adults due to a combination of factors. Key considerations include:
Age-Related Changes: As individuals age, they may experience changes in body composition, including increased fat mass and decreased muscle mass, contributing to insulin resistance.
Comorbidities: Older adults often have multiple chronic conditions, which can complicate the management of metabolic diseases.
The Role of Prevention
Early Detection and Screening
Early detection of metabolic diseases is crucial for effective management and prevention of complications. Regular screening for conditions such as obesity, diabetes, and dyslipidemia can help identify individuals at risk and promote timely interventions.
Lifestyle Interventions
Implementing lifestyle interventions is essential for preventing the onset of metabolic diseases. Key strategies include:
Healthy Eating: Encouraging a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain a healthy weight and improve metabolic health.
Physical Activity: Promoting regular physical activity can help individuals maintain a healthy weight, improve insulin sensitivity, and reduce the risk of metabolic diseases.
Behavioral Support: Providing support and resources for individuals to make sustainable lifestyle changes can enhance the effectiveness of prevention efforts.
Community and Policy Initiatives
Community and policy initiatives play a vital role in promoting metabolic health. Key initiatives include:
Access to Healthy Foods: Improving access to affordable, healthy food options in underserved communities can help reduce the prevalence of metabolic diseases.
Physical Activity Opportunities: Creating safe environments for physical activity, such as parks and recreational facilities, can encourage individuals to engage in regular exercise.
Public Health Campaigns: Raising awareness about the importance of metabolic health and promoting healthy lifestyle choices through public health campaigns can help reduce the incidence of metabolic diseases.
Conclusion
Metabolic diseases are complex conditions influenced by a variety of factors, including genetics, age, lifestyle, environment, and psychological well-being. Understanding when metabolic diseases occur is essential for effective prevention and management.
The onset of these diseases can begin in childhood and continue into older adulthood, with lifestyle choices playing a significant role at every stage. By promoting healthy eating, regular physical activity, and early detection, we can reduce the prevalence of metabolic diseases and improve overall health outcomes.
As we continue to learn more about the factors contributing to metabolic diseases, it is crucial to implement community and policy initiatives that support healthy lifestyles and provide access to resources for individuals at risk. Through collaborative efforts, we can work towards a healthier future and mitigate the impact of metabolic diseases on individuals and society as a whole.
Related Topics: