Junctional bradycardia is a type of arrhythmia, a condition where the heart beats irregularly or too slowly. Specifically, it refers to a slow heart rate that originates from the junction of the atria and ventricles, known as the atrioventricular (AV) junction. The condition is characterized by a heart rate that is slower than normal, typically less than 60 beats per minute, due to disturbances in the electrical conduction system of the heart.
Unlike normal heart rhythm, which is controlled by the sinoatrial (SA) node, the natural pacemaker of the heart, junctional bradycardia arises when the AV junction assumes the role of pacing the heart. This can happen due to a variety of reasons, ranging from age-related changes to heart disease, electrolyte imbalances, or even the use of certain medications.
In this article, we will explore the causes, symptoms, diagnosis, and treatment options for junctional bradycardia. We will also discuss the potential risks associated with the condition and provide guidance on when medical intervention is necessary.
1. What is Junctional Bradycardia?
Junctional bradycardia occurs when the electrical signals that regulate the heart’s rhythm originate from the AV junction rather than the SA node. The AV junction, located at the intersection of the atria and ventricles, can take over as the heart’s pacemaker when the SA node fails to function properly. However, the pacing rate from the AV junction is slower than the typical 60 to 100 beats per minute, resulting in bradycardia, or a slow heart rate.
How Does the Heart Normally Beat?
To understand junctional bradycardia, it is essential to understand how the heart typically beats. Under normal circumstances, electrical signals are generated in the SA node, which is located in the right atrium. These electrical impulses travel through the atria, causing them to contract and pump blood into the ventricles. The signals then pass through the AV node, which acts as a gateway to the ventricles, and finally reach the bundle of His and Purkinje fibers, triggering ventricular contraction.
In the case of junctional bradycardia, the electrical signals originate from the AV junction, which results in a slower heart rate. This is often the result of malfunctioning or delayed signals from the SA node, and in some cases, the electrical impulses may not reach the ventricles effectively.
2. Causes of Junctional Bradycardia
Junctional bradycardia can be caused by several factors, including heart conditions, medications, electrolyte imbalances, and other underlying health issues. Below are some of the most common causes:
Heart Disease
Various heart conditions can lead to junctional bradycardia. Some of the most common heart-related causes include:
Sick Sinus Syndrome: This condition refers to the malfunctioning of the SA node, leading to a slow or irregular heart rate.
In cases of sick sinus syndrome, the AV junction may take over as the pacemaker, resulting in junctional bradycardia.
Heart Attack: Damage to the heart muscle during a heart attack can disrupt the normal electrical pathways, which can lead to junctional bradycardia. This is especially common when the electrical conduction system is directly affected.
Heart Valve Disease: If the heart valves are damaged or diseased, the electrical conduction system can be affected, leading to arrhythmias, including junctional bradycardia.
Coronary Artery Disease: Blockages in the coronary arteries can limit blood flow to the heart muscle, leading to ischemia. Ischemia can impair the heart’s ability to generate normal electrical signals, potentially resulting in junctional bradycardia.
Medications
Certain medications can also cause junctional bradycardia as a side effect. These include:
Beta-blockers: Beta-blockers are commonly prescribed for high blood pressure, heart failure, and arrhythmias. While effective in managing these conditions, they can slow the heart rate, leading to bradycardia.
Calcium Channel Blockers: These medications, used to treat high blood pressure and heart-related issues, can also slow the heart rate and lead to junctional bradycardia.
Digoxin: A medication often used to treat heart failure and arrhythmias, digoxin can slow down the heart rate, leading to junctional bradycardia in some cases.
Electrolyte Imbalances
Electrolytes are essential for the proper functioning of the heart, as they regulate electrical signals. Imbalances in electrolytes, such as potassium, calcium, and magnesium, can disrupt the normal heart rhythm and contribute to junctional bradycardia.
Hypokalemia (Low Potassium): Low potassium levels can impair the heart’s ability to generate electrical signals, leading to bradycardia and other arrhythmias.
Hypocalcemia (Low Calcium): A deficiency in calcium can also disrupt the normal electrical conduction in the heart, causing bradycardia.
Other Health Conditions
Hypothyroidism: An underactive thyroid gland can cause a variety of symptoms, including a slow heart rate. Low thyroid hormone levels can slow down the electrical signals in the heart, potentially resulting in junctional bradycardia.
Sleep Apnea: People with sleep apnea may experience drops in heart rate during episodes of airway obstruction. This can sometimes result in junctional bradycardia.
Aging: As people age, the electrical conduction system in the heart can naturally become less efficient. This can result in bradycardia, including junctional bradycardia.
3. Symptoms of Junctional Bradycardia
Junctional bradycardia can present a wide range of symptoms, depending on the severity of the condition and the underlying cause. Some individuals may experience no symptoms at all, while others may have more pronounced effects on their daily activities. Common symptoms of junctional bradycardia include:
Fatigue
A slow heart rate means the heart is pumping less blood and oxygen to the body’s tissues and organs. As a result, individuals with junctional bradycardia may feel unusually tired or fatigued, especially during physical activities.
Dizziness or Lightheadedness
A slower heart rate can affect blood flow to the brain, causing dizziness or lightheadedness. This is particularly noticeable when standing up quickly or engaging in physical activity.
Fainting (Syncope)
In more severe cases of junctional bradycardia, blood flow to the brain may become insufficient, leading to fainting or near-fainting episodes. This can occur suddenly and without warning.
Shortness of Breath
A slower heart rate can reduce the heart’s ability to pump oxygenated blood effectively to the lungs and other organs. As a result, individuals may experience shortness of breath or difficulty breathing, especially during physical exertion.
Chest Pain
In some cases, junctional bradycardia may lead to chest discomfort or pain, particularly if the condition is associated with underlying heart disease or ischemia.
Exercise Intolerance
People with junctional bradycardia may find it difficult to engage in physical activity, as their hearts are not pumping blood efficiently enough to meet the demands of exercise. This may lead to fatigue, breathlessness, and other symptoms during physical exertion.
4. Diagnosis of Junctional Bradycardia
If junctional bradycardia is suspected, a healthcare provider will typically perform a physical examination and take a thorough medical history. The following tests may be used to diagnose junctional bradycardia:
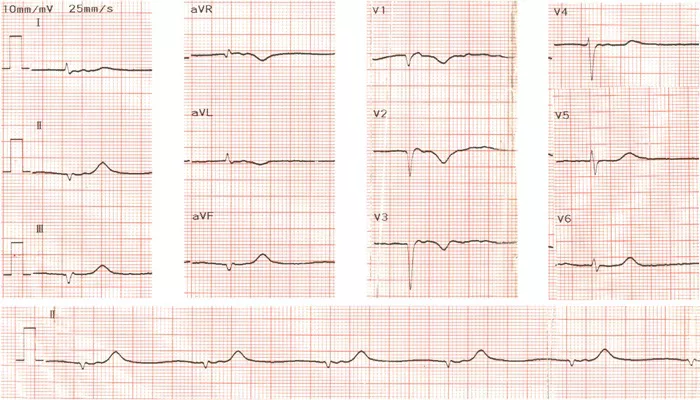
Electrocardiogram (ECG)
An ECG is the primary diagnostic tool for detecting arrhythmias, including junctional bradycardia. This test records the electrical activity of the heart and can show the specific heart rhythm and whether it originates from the AV junction. The ECG will also provide information about the heart rate and the regularity of the beats.
Holter Monitor
A Holter monitor is a portable ECG device worn for 24 to 48 hours to monitor the heart’s rhythm over a longer period. This test can detect intermittent arrhythmias that may not appear during a standard ECG.
Echocardiogram
An echocardiogram uses sound waves to create an image of the heart’s structure and function. This test can help identify underlying heart conditions that may be contributing to junctional bradycardia, such as heart valve disease or damage from a heart attack.
5. Treatment of Junctional Bradycardia
The treatment for junctional bradycardia depends on the severity of the condition and the underlying cause. In many cases, treatment may not be necessary if the bradycardia is mild and asymptomatic. However, for more severe cases, the following treatment options may be considered:
Medication Adjustments
If the bradycardia is caused by medications such as beta-blockers or calcium channel blockers, the healthcare provider may adjust the dosage or switch to alternative medications. In some cases, discontinuing the offending medication may resolve the issue.
Pacemaker
In cases of severe junctional bradycardia, especially when it causes symptoms such as fainting or exercise intolerance, a pacemaker may be required. A pacemaker is a small device implanted under the skin that sends electrical signals to regulate the heart’s rhythm and ensure it beats at an appropriate rate.
Management of Underlying Conditions
If junctional bradycardia is caused by an underlying condition, such as hypothyroidism or electrolyte imbalances, treating the root cause can often improve or resolve the bradycardia. For example, thyroid hormone replacement therapy may be prescribed for hypothyroidism, or electrolyte supplements may be used to correct imbalances.
Lifestyle Changes
In some cases, lifestyle changes such as increasing physical activity, improving diet, and managing stress may help improve heart health and reduce the symptoms of junctional bradycardia.
Conclusion
Junctional bradycardia is a condition in which the heart beats too slowly due to electrical disturbances in the AV junction. It can be caused by a variety of factors, including heart disease, medication use, electrolyte imbalances, and aging. Symptoms can vary, but common signs include fatigue, dizziness, fainting, and shortness of breath. Diagnosis typically involves an ECG and other tests, while treatment may include medication adjustments, pacemaker implantation, and management of underlying conditions.
Related topics: