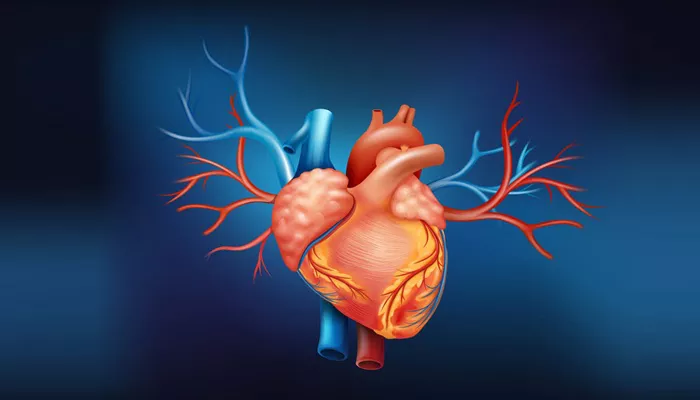
Diastolic dysfunction refers to a condition in which the heart’s ability to relax and fill with blood during the diastolic phase (the phase when the heart relaxes between beats) is impaired. This dysfunction typically occurs in the left ventricle, the chamber of the heart responsible for pumping oxygen-rich blood throughout the body. Mild diastolic dysfunction is a common finding in many individuals, particularly as they age. Although it is often seen as a precursor to heart failure, it does not always lead to severe complications. Understanding its symptoms, causes, and treatment options is crucial for managing the condition effectively.
What is Mild Diastolic Dysfunction?
Mild diastolic dysfunction occurs when there is a slight impairment in the heart’s ability to relax and fill properly during diastole. This condition is typically identified during an echocardiogram, a non-invasive imaging test that uses sound waves to produce images of the heart. Diastolic dysfunction is graded into stages, with mild dysfunction being the least severe. While the heart can still pump blood effectively, the reduced ability to fill with blood during relaxation can sometimes lead to symptoms such as shortness of breath, fluid retention, and fatigue.
It is essential to note that mild diastolic dysfunction is different from diastolic heart failure (also known as heart failure with preserved ejection fraction, or HFpEF), which is a more severe condition where the heart is unable to pump blood effectively due to impaired relaxation and filling.
Causes of Mild Diastolic Dysfunction
Mild diastolic dysfunction can arise from a variety of factors. It may develop gradually and is often associated with aging, but several medical conditions can also contribute to its onset. Below are some of the most common causes:
1. Aging
As individuals age, the heart muscle naturally becomes stiffer. This stiffness reduces the heart’s ability to relax properly during diastole, impairing its filling capacity. Mild diastolic dysfunction is frequently seen in older adults as a part of the aging process. The condition may not present with overt symptoms initially, but over time, it can lead to other heart problems.
2. Hypertension (High Blood Pressure)
Chronic high blood pressure puts extra strain on the heart. The left ventricle, in particular, has to work harder to overcome the increased resistance, leading to the thickening of the heart muscle (left ventricular hypertrophy). This thickening can cause stiffness in the left ventricle, impairing its ability to relax properly during diastole, thus leading to diastolic dysfunction.
3. Coronary Artery Disease (CAD)
Coronary artery disease, which is caused by the buildup of plaque in the coronary arteries, can impair blood flow to the heart muscle. Reduced blood supply can lead to changes in the structure and function of the heart muscle, contributing to diastolic dysfunction. CAD often coexists with other risk factors, such as hypertension and diabetes, which further exacerbate the condition.
4. Obesity
Obesity has been associated with increased risk factors for diastolic dysfunction, including hypertension, diabetes, and sleep apnea. Excess weight puts additional strain on the heart, and the resultant changes in the heart muscle can impair diastolic function. In individuals with obesity, the risk of developing heart failure with preserved ejection fraction (HFpEF) is notably higher.
5. Diabetes
Diabetes, particularly when poorly controlled, can contribute to diastolic dysfunction in several ways. High blood sugar levels can damage blood vessels and the heart muscle, leading to stiffening of the heart tissue and impairing diastolic function. Diabetic cardiomyopathy is a term used to describe heart dysfunction that occurs as a result of long-term diabetes.
6. Valvular Heart Disease
Certain heart valve conditions, such as aortic stenosis (narrowing of the aortic valve) or mitral regurgitation (leakage of the mitral valve), can lead to diastolic dysfunction. When the heart valves do not function properly, the pressure within the heart chambers increases, leading to structural changes and impaired diastolic relaxation.
7. Other Conditions
Other conditions that can contribute to mild diastolic dysfunction include chronic kidney disease, certain inflammatory conditions like rheumatoid arthritis, and excessive alcohol consumption. Additionally, smoking and a sedentary lifestyle are known risk factors for heart disease that can also affect diastolic function.
Symptoms of Mild Diastolic Dysfunction
Mild diastolic dysfunction does not always cause noticeable symptoms, especially in the early stages. In many cases, individuals may not even be aware they have the condition unless they undergo imaging tests like echocardiograms.
However, when symptoms do arise, they are often related to the heart’s reduced ability to relax and fill properly. Some of the most common symptoms include:
1. Shortness of Breath (Dyspnea)
One of the hallmark symptoms of diastolic dysfunction is shortness of breath, particularly during physical activity or when lying flat. This occurs because the heart struggles to fill with blood effectively, which can lead to fluid buildup in the lungs (pulmonary congestion). When fluid accumulates in the lungs, it causes difficulty breathing and a sensation of breathlessness.
2. Fatigue
Individuals with mild diastolic dysfunction may experience unexplained fatigue or a general feeling of tiredness. The heart’s reduced ability to fill with blood and supply oxygenated blood to the body can lead to decreased energy levels, making it harder for individuals to perform daily activities.
3. Swelling (Edema)
Fluid retention is another common symptom, particularly in the legs, ankles, and feet. As the heart becomes less efficient at filling and pumping blood, fluid can accumulate in the lower extremities, causing swelling. This condition is known as peripheral edema.
4. Chest Discomfort or Pain
Some individuals with diastolic dysfunction may experience chest discomfort, which can be related to a variety of factors, including reduced oxygen supply to the heart muscle or the increased workload on the heart. However, chest pain is not as common in mild diastolic dysfunction and may be indicative of more severe heart conditions.
5. Palpitations
Palpitations, or the sensation of an irregular heartbeat, may occur as the heart tries to compensate for the reduced filling.
These irregular rhythms can sometimes be noticeable, especially during physical exertion or emotional stress.
6. Sleep Disturbances
Many individuals with diastolic dysfunction also suffer from sleep disturbances, such as sleep apnea. This is partly due to the fluid buildup in the lungs, which makes it difficult for individuals to breathe easily while sleeping.
Treatment of Mild Diastolic Dysfunction
While mild diastolic dysfunction does not always require aggressive treatment, addressing the underlying causes and managing symptoms can help prevent the progression to more severe heart failure. The treatment plan typically includes lifestyle changes, medications, and regular monitoring.
1. Lifestyle Modifications
Lifestyle changes are often the first line of defense in managing mild diastolic dysfunction. Key lifestyle modifications include:
Weight management: Achieving and maintaining a healthy weight can reduce the strain on the heart and improve diastolic function.
Regular exercise: Engaging in regular physical activity can help improve cardiovascular health, reduce blood pressure, and promote overall heart function. However, individuals should consult their doctor before starting any exercise program.
Dietary changes: A heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help control blood pressure and cholesterol levels, reducing the risk of worsening diastolic dysfunction.
Limiting alcohol and smoking cessation: Reducing alcohol intake and quitting smoking can significantly improve heart health and prevent further damage to the heart.
2. Medications
Several medications may be prescribed to help manage symptoms and underlying conditions that contribute to diastolic dysfunction:
ACE inhibitors and ARBs: These medications are often used to lower blood pressure and reduce the workload on the heart.
They can also help reduce the stiffness in the heart muscle, improving diastolic function.
Beta-blockers: Beta-blockers help slow the heart rate and reduce the heart’s oxygen demand, which can be helpful in managing diastolic dysfunction caused by high blood pressure or coronary artery disease.
Diuretics: If fluid retention is a problem, diuretics may be prescribed to help remove excess fluid from the body, reducing swelling and shortness of breath.
Calcium channel blockers: These medications may be used to help relax the heart muscle and improve diastolic function, especially in patients with hypertension.
3. Managing Underlying Conditions
Effective management of underlying conditions such as hypertension, diabetes, and coronary artery disease is crucial in preventing further deterioration of heart function. This may include controlling blood sugar levels, managing cholesterol, and reducing the risks associated with these conditions.
4. Regular Monitoring
Individuals with mild diastolic dysfunction should have regular check-ups with their healthcare provider to monitor heart function and adjust treatment plans as needed. Regular echocardiograms and other tests can help track the progression of the condition.
Conclusion
Mild diastolic dysfunction is a common heart condition that affects many individuals, particularly as they age. Although it may not always cause severe symptoms, it can lead to complications if left untreated. Understanding the causes, recognizing the symptoms, and implementing appropriate treatment strategies can help manage the condition effectively.
With lifestyle changes, medications, and regular monitoring, many individuals with mild diastolic dysfunction can maintain good heart health and prevent further complications.
Related topics: