Arrhythmic Right Ventricular Cardiomyopathy (ARVC) is a rare but serious heart condition that affects the right ventricle, the lower chamber of the heart responsible for pumping deoxygenated blood to the lungs. It is characterized by the progressive replacement of healthy heart muscle tissue with fatty or fibrous tissue, which interferes with the heart’s ability to contract and conduct electrical signals properly. As the name suggests, ARVC primarily affects the right side of the heart but can extend to the left ventricle in more advanced stages of the disease.
ARVC is a type of cardiomyopathy, a group of diseases that affect the heart muscle, and it is considered a major cause of arrhythmias, particularly ventricular arrhythmias, which can be life-threatening. It can lead to sudden cardiac death, especially in younger individuals, making early diagnosis and treatment crucial for improving outcomes.
This article will provide an in-depth look at ARVC, including its causes, symptoms, diagnosis, and treatment options. We will also discuss the risks associated with the condition and the importance of lifestyle changes and medical management in controlling symptoms and preventing complications.
1. What is Arrhythmic Right Ventricular Cardiomyopathy (ARVC)?
Arrhythmic Right Ventricular Cardiomyopathy (ARVC) is a heart disease that primarily affects the right ventricle, but it may also involve other chambers of the heart. It is characterized by the replacement of healthy heart muscle with fibrous or fatty tissue, which disrupts the normal function of the heart. The condition causes abnormal electrical activity in the heart, leading to arrhythmias, particularly ventricular arrhythmias, which are irregularities in the heart’s rhythm that originate in the ventricles.
The condition often goes undiagnosed for many years due to its gradual progression and the absence of early symptoms. ARVC is typically inherited in an autosomal dominant pattern, meaning that one copy of the altered gene in each cell is sufficient to cause the disorder. Although it primarily affects young adults, it can occur at any age.
How Does ARVC Affect the Heart?
In a healthy heart, the muscle fibers contract and relax in a coordinated manner to pump blood efficiently. However, in ARVC, the heart muscle fibers in the right ventricle are gradually replaced with fatty or fibrous tissue. This disruption can interfere with the heart’s ability to pump blood effectively and can lead to electrical abnormalities.
The abnormal tissue replacement in ARVC disrupts the normal conduction of electrical signals, leading to arrhythmias such as ventricular tachycardia (VT) and ventricular fibrillation (VF). These arrhythmias can cause a fast, irregular heart rate, which reduces the heart’s ability to pump blood effectively, potentially leading to symptoms such as dizziness, fainting, or even sudden cardiac arrest.
2. Causes of ARVC
ARVC is often caused by genetic mutations that affect the proteins responsible for maintaining the structure and function of the heart muscle. These genetic mutations are typically inherited, meaning that individuals with a family history of ARVC are at higher risk of developing the condition. However, in some cases, the condition may occur without a clear family history, and the cause may be related to spontaneous genetic mutations.
Genetic Mutations
Most cases of ARVC are linked to mutations in genes that code for desmosomal proteins. These proteins play a crucial role in holding heart muscle cells together and maintaining the structure of the heart. When these proteins are defective or absent, the structural integrity of the heart muscle is compromised, leading to the development of fatty or fibrous tissue in the affected areas. The most common genes associated with ARVC include:
- Desmoglein-2 (DSG2)
- Desmocollin-2 (DSC2)
- Plakophilin-2 (PKP2)
- Desmoplakin (DSP)
Mutations in these genes disrupt the desmosomal junctions between heart muscle cells, leading to the accumulation of fatty or fibrous tissue. This abnormal tissue replaces healthy muscle and creates electrical disturbances that increase the risk of arrhythmias.
Autosomal Dominant Inheritance
ARVC is most commonly inherited in an autosomal dominant manner, meaning that an individual needs only one copy of the mutated gene from either parent to develop the condition. However, the severity and age of onset of the disease can vary widely, even among family members with the same genetic mutation. In some cases, ARVC may be inherited in a recessive pattern, meaning that an individual would need to inherit two copies of the defective gene (one from each parent) to develop the condition.
Environmental Factors and Other Triggers
While genetic mutations play a central role in the development of ARVC, environmental factors and other triggers may also contribute to the progression of the disease. Some potential triggers for ARVC symptoms include:
Intense physical activity: Athletes, especially those who engage in endurance sports or intense training, may experience an increased risk of developing arrhythmias in individuals with a genetic predisposition to ARVC. This phenomenon is thought to be linked to changes in the heart muscle resulting from prolonged physical exertion.
Infections: In some cases, viral infections affecting the heart (such as viral myocarditis) may trigger or exacerbate the progression of ARVC, particularly in individuals with an underlying genetic predisposition.
Other heart conditions: Conditions such as heart failure or coronary artery disease may worsen the effects of ARVC by further impairing heart function and electrical conduction.
3. Symptoms of ARVC
The symptoms of ARVC can vary widely depending on the severity of the condition and the extent of the heart muscle damage. Many individuals with ARVC may not experience symptoms until later stages of the disease, and symptoms may initially be mild or intermittent. However, over time, the condition can progress and cause significant symptoms that impact the individual’s quality of life.
Ventricular Arrhythmias
One of the hallmark features of ARVC is the development of abnormal heart rhythms, particularly ventricular arrhythmias such as ventricular tachycardia (VT) and ventricular fibrillation (VF). These arrhythmias are caused by electrical disturbances in the heart, which can lead to:
Palpitations: A sensation of a racing or irregular heartbeat.
Dizziness or Lightheadedness: Caused by the heart’s inability to pump blood effectively during arrhythmias.
Fainting (Syncope): Loss of consciousness due to insufficient blood flow to the brain during arrhythmias.
Heart Failure Symptoms
As ARVC progresses, the damage to the heart muscle may impair the heart’s ability to pump blood efficiently. This can lead to symptoms of heart failure, including:
Shortness of breath: Difficulty breathing, particularly during physical exertion or while lying flat.
Fatigue: Feeling unusually tired or weak, even with minimal activity.
Swelling (Edema): Swelling in the legs, ankles, or abdomen due to fluid retention.
Sudden Cardiac Arrest (SCA)
In severe cases of ARVC, individuals may experience sudden cardiac arrest, which is a life-threatening condition that occurs when the heart stops beating. This is often caused by ventricular fibrillation, a chaotic and ineffective heart rhythm that can lead to death if not treated immediately. Sudden cardiac arrest is one of the leading causes of death in young athletes with ARVC, making early detection and management critical.
4. Diagnosis of ARVC
Diagnosing ARVC can be challenging due to its gradual progression and the variability of symptoms. The diagnosis is typically made based on a combination of clinical evaluation, family history, imaging tests, and genetic testing.
Electrocardiogram (ECG)
An ECG is a common test used to assess the electrical activity of the heart. In individuals with ARVC, the ECG may show signs of arrhythmias, including ventricular tachycardia, which can suggest the presence of the condition.
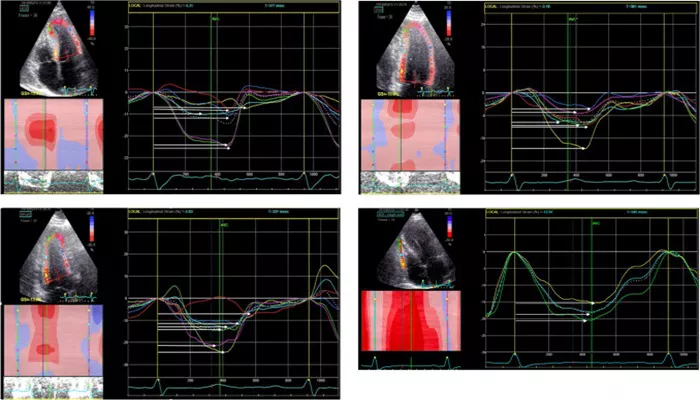
Echocardiogram
An echocardiogram uses ultrasound waves to create images of the heart’s structure and function. It can help identify abnormalities in the heart’s size, shape, and movement, which may indicate ARVC. However, an echocardiogram may not always detect early-stage ARVC.
Cardiac MRI
Cardiac MRI is a more advanced imaging technique that can provide detailed images of the heart’s tissue and structures. It is particularly useful in detecting fatty or fibrous tissue replacement in the right ventricle, which is characteristic of ARVC.
Genetic Testing
Genetic testing can help identify mutations in genes associated with ARVC. If a genetic mutation is detected, it can confirm the diagnosis and provide important information about the risk of the condition in other family members.
Endomyocardial Biopsy
In rare cases, a biopsy of the heart tissue may be performed to examine the extent of the damage and confirm the presence of fatty or fibrous tissue replacement. However, this procedure is typically reserved for cases where the diagnosis is unclear.
5. Treatment of ARVC
While there is no cure for ARVC, treatment aims to manage symptoms, reduce the risk of arrhythmias, and improve the patient’s quality of life. Treatment options may include medications, lifestyle modifications, and medical devices.
Medications
Antiarrhythmic Drugs: These medications can help control abnormal heart rhythms and prevent life-threatening arrhythmias.
Beta-Blockers: Beta-blockers are commonly prescribed to reduce the heart rate and prevent arrhythmias in individuals with ARVC.
Anti-coagulants: In some cases, anticoagulants (blood thinners) may be prescribed to reduce the risk of blood clots, especially if the individual has atrial fibrillation.
Implantable Cardioverter-Defibrillator (ICD)
An ICD is a device implanted under the skin that continuously monitors the heart’s rhythm. If the ICD detects a life-threatening arrhythmia, it delivers an electric shock to restore normal heart rhythm. This is particularly important for individuals at high risk of sudden cardiac arrest.
Catheter Ablation
Catheter ablation is a procedure used to treat arrhythmias by destroying the abnormal tissue that is causing the electrical disturbances. It may be used in individuals with persistent arrhythmias that do not respond to medications.
Heart Transplant
In severe cases where heart failure progresses and other treatments are ineffective, a heart transplant may be considered.
However, this is typically a last-resort option for individuals with advanced ARVC.
6. Lifestyle Changes and Prevention
Although there is no cure for ARVC, certain lifestyle changes can help manage the condition and reduce the risk of complications:
Avoid Intense Physical Activity: Individuals with ARVC should avoid activities that place excessive strain on the heart, particularly high-intensity sports or exercise.
Maintain a Healthy Diet: A balanced diet rich in fruits, vegetables, and lean proteins can help support heart health and prevent complications.
Regular Monitoring: Regular follow-up appointments with a cardiologist are essential to monitor heart function, detect arrhythmias, and adjust treatment as needed.
Conclusion
Arrhythmic Right Ventricular Cardiomyopathy is a rare but serious heart condition that can lead to life-threatening arrhythmias and sudden cardiac arrest. Early diagnosis and treatment are crucial to managing symptoms and preventing complications. While there is no cure for ARVC, a combination of medications, lifestyle changes, and medical devices such as ICDs can help improve quality of life and reduce the risk of sudden cardiac events.
Related topics: