Diastolic dysfunction is a condition where the heart’s ability to relax and fill with blood during the diastolic phase of the cardiac cycle is impaired. This dysfunction can range from mild to severe, with moderate diastolic dysfunction sitting in between. While mild diastolic dysfunction may not present significant symptoms, moderate diastolic dysfunction can be more pronounced and may lead to notable clinical manifestations, such as shortness of breath, fatigue, and fluid retention. This condition is often associated with heart failure, particularly heart failure with preserved ejection fraction (HFpEF).
Moderate diastolic dysfunction occurs when the left ventricle becomes less compliant, meaning it is less able to expand and fill with blood efficiently. The increased pressure in the heart due to this decreased compliance can cause symptoms of congestion in various organs, particularly the lungs. Understanding the causes, symptoms, and treatment options for moderate diastolic dysfunction is essential for managing the condition and preventing it from progressing into more severe forms of heart disease.
In this article, we will explore the causes, symptoms, and treatment strategies for moderate diastolic dysfunction in detail. By understanding the pathophysiology of this condition, as well as its clinical impact, individuals can better manage the symptoms and reduce the risk of complications.
What is Moderate Diastolic Dysfunction?
Moderate diastolic dysfunction refers to an impairment in the relaxation phase of the heart’s pumping action, specifically during the diastole phase when the heart fills with blood. In a healthy heart, the left ventricle relaxes and fills with blood coming from the lungs. However, in diastolic dysfunction, the left ventricle becomes stiff and less compliant, making it more difficult for blood to fill the ventricle adequately.
Moderate diastolic dysfunction is characterized by:
Decreased left ventricular compliance: The heart’s left ventricle becomes stiffer, and the walls are less able to relax and expand as blood flows into the heart.
Increased filling pressures: As a result of the decreased compliance, the left atrium and pulmonary veins experience increased pressure, which can cause fluid to accumulate in the lungs and other parts of the body.
Impaired relaxation: The heart struggles to relax after contracting, which can lead to an insufficient filling of the ventricle.
This type of dysfunction is often diagnosed through echocardiography, which measures the filling pressures and diastolic function of the heart.
Causes of Moderate Diastolic Dysfunction
Moderate diastolic dysfunction can occur due to a variety of underlying conditions that affect the heart’s ability to relax and fill properly. These causes are generally related to increased stiffness in the heart’s left ventricle or conditions that increase the workload on the heart. The most common causes of moderate diastolic dysfunction include:
1. Hypertension (High Blood Pressure)
Chronic hypertension is one of the most significant risk factors for diastolic dysfunction. Over time, high blood pressure can cause the heart’s left ventricle to work harder to pump blood, which leads to thickening of the heart muscle (left ventricular hypertrophy). This thickening reduces the heart’s ability to relax and fill properly during diastole, causing the development of diastolic dysfunction.
The persistent high pressure in the arteries forces the heart to pump against increased resistance, leading to the stiffening of the heart walls. This ultimately leads to both moderate diastolic dysfunction and an increased risk of heart failure with preserved ejection fraction (HFpEF).
2. Aging
As individuals age, the heart’s tissues naturally become stiffer due to the accumulation of collagen and other fibrous tissue in the heart muscle. This results in reduced compliance of the left ventricle, making it less able to relax and fill efficiently during diastole. Aging is one of the most common factors contributing to moderate diastolic dysfunction, especially in people over 60.
3. Coronary Artery Disease (CAD)
Coronary artery disease, which is characterized by the buildup of plaque in the coronary arteries, can reduce blood flow to the heart muscle, leading to ischemia (a lack of oxygen). Over time, this reduced oxygen supply can lead to scarring and stiffness in the heart muscle, contributing to moderate diastolic dysfunction. CAD can also cause changes in the structure and function of the left ventricle, worsening diastolic dysfunction.
4. Diabetes and Metabolic Syndrome
Diabetes and metabolic syndrome are associated with increased inflammation, oxidative stress, and changes in blood vessel function.
These conditions can lead to stiffening of the heart’s left ventricle and increased left atrial pressure, resulting in diastolicdysfunction. Moreover, diabetes can contribute to the development of coronary artery disease, further exacerbating the risk of diastolic dysfunction.
5. Obesity
Obesity is a major risk factor for both hypertension and metabolic syndrome, both of which contribute to diastolic dysfunction. Excess body fat, especially abdominal fat, can lead to increased inflammation and changes in the structure of the heart, leading to diastolic dysfunction. Furthermore, obesity is a major risk factor for heart failure with preserved ejection fraction (HFpEF), a condition that commonly occurs alongside moderate diastolic dysfunction.
6. Valvular Heart Disease
Certain conditions that affect the heart valves, such as mitral valve stenosis (narrowing) or aortic valve disease, can result in increased pressures within the heart. These conditions can increase the workload on the heart and lead to stiffening of the left ventricle, contributing to moderate diastolic dysfunction. In particular, mitral valve stenosis can cause elevated left atrial pressure, which can impair the left ventricle’s ability to relax and fill with blood.
7. Chronic Kidney Disease
Chronic kidney disease (CKD) is closely associated with cardiovascular dysfunction. It can lead to increased fluid retention, increased blood pressure, and changes in the heart’s structure, contributing to diastolic dysfunction. The kidneys help regulate blood volume and pressure, and when they are not functioning properly, they can exacerbate the strain on the heart.
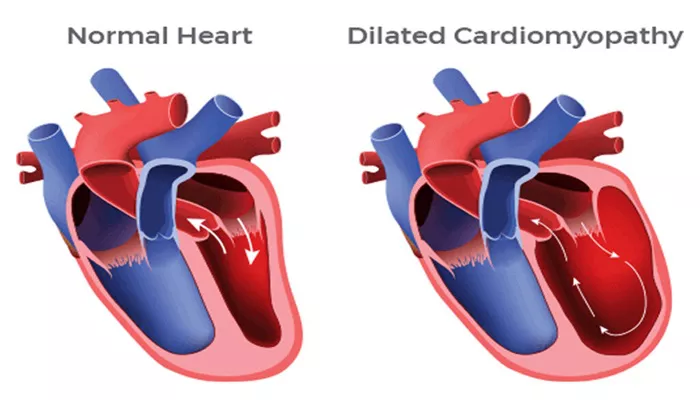
8. Inflammatory Conditions and Cardiomyopathies
Certain inflammatory conditions, such as myocarditis (inflammation of the heart muscle), and specific forms of cardiomyopathy, can cause scarring and stiffness of the heart muscle. This can lead to impaired diastolic function. These conditions often lead to heart failure and can worsen diastolic dysfunction, making it important to monitor and treat them appropriately.
Symptoms of Moderate Diastolic Dysfunction
The symptoms of moderate diastolic dysfunction often result from the increased pressure in the left atrium and pulmonary veins due to impaired filling of the left ventricle. These symptoms are often associated with heart failure and can vary in severity based on the underlying cause and the stage of the disease. Common symptoms of moderate diastolic dysfunction include:
1. Shortness of Breath (Dyspnea)
One of the most common symptoms of moderate diastolic dysfunction is shortness of breath, particularly with physical activity or when lying down (orthopnea). Fluid backs up into the lungs as a result of increased pressure in the pulmonary circulation, impairing the lungs’ ability to oxygenate the blood. This can cause significant difficulty in breathing.
2. Fatigue
As the heart is unable to pump blood effectively, individuals with moderate diastolic dysfunction may experience fatigue and reduced exercise tolerance. Decreased oxygen delivery to the muscles and tissues can lead to persistent tiredness and a lack of energy, even after adequate rest.
3. Swelling (Edema)
Fluid retention is a common symptom of diastolic dysfunction, especially in the lower extremities (legs, ankles, and feet).
When the left ventricle is unable to pump blood efficiently, blood backs up into the veins, leading to fluid accumulation.
This may also manifest as abdominal swelling or a feeling of fullness.
4. Chest Discomfort
Some individuals with moderate diastolic dysfunction may experience chest discomfort, which can be due to increased pressure in the heart or ischemia resulting from coronary artery disease. While chest pain may not always be severe, it is important to monitor for any discomfort in the chest, particularly if it is associated with shortness of breath.
5. Cough
A persistent cough, particularly one that produces pink-tinged sputum, is a common symptom of pulmonary congestion associated with diastolic dysfunction. The fluid buildup in the lungs irritates the airways, leading to coughing.
6. Rapid Heartbeat (Tachycardia)
To compensate for reduced cardiac output, the heart may increase its rate of beating. This tachycardia (rapid heartbeat) is a common symptom of heart failure, including moderate diastolic dysfunction.
The rapid heartbeat may be noticeable to the individual and can contribute to feelings of palpitations or irregular heart rhythms.
Treatment of Moderate Diastolic Dysfunction
The treatment of moderate diastolic dysfunction focuses on addressing the underlying causes, relieving symptoms, and improving the heart’s ability to function properly. Treatment typically involves medications, lifestyle changes, and, in some cases, surgical interventions. The primary goal is to manage the condition and prevent it from progressing into severe heart failure.
1. Medications
Several types of medications are used to manage moderate diastolic dysfunction, including:
Diuretics: These medications help reduce fluid buildup in the body and alleviate symptoms of congestion, such as swelling and shortness of breath.
ACE Inhibitors or ARBs: Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers help relax blood vessels, lower blood pressure, and reduce the workload on the heart. These are commonly used in individuals with hypertension and diastolic dysfunction.
Beta-Blockers: Beta-blockers are used to reduce the heart rate and lower blood pressure, which helps decrease the workload on the heart and improves diastolic function.
Calcium Channel Blockers: These medications help relax the heart’s muscle and blood vessels, improving the heart’s ability to fill with blood during diastole.
Aldosterone Antagonists: In patients with heart failure or hypertension, aldosterone antagonists can be used to prevent fluid retention and reduce the strain on the heart.
2. Lifestyle Modifications
Lifestyle changes are crucial for managing moderate diastolic dysfunction. These include:
Dietary Changes: Reducing sodium intake and following a heart-healthy diet can help manage blood pressure and prevent fluid retention.
Exercise: Regular physical activity is beneficial for improving cardiovascular health, although it should be tailored to the individual’s level of fitness and coordinated with their healthcare provider.
Weight Management: Maintaining a healthy weight can reduce the strain on the heart and help prevent the progression of diastolic dysfunction.
3. Monitoring and Follow-Up Care
Regular follow-up care is essential for individuals with moderate diastolic dysfunction. This typically involves monitoring heart function, blood pressure, and symptoms through routine clinical exams, echocardiography, and blood tests.
Monitoring allows for adjustments in medications and lifestyle recommendations to ensure optimal management of the condition.
4. Surgical Interventions
In cases where the underlying cause is related to valvular heart disease or coronary artery disease, surgical interventions may be necessary.
These may include valve repair or replacement, or coronary artery bypass surgery to improve blood flow to the heart.
Conclusion
Moderate diastolic dysfunction is a condition that can significantly affect an individual’s quality of life and overall cardiovascular health. By understanding the causes, recognizing the symptoms, and implementing appropriate treatments, individuals with moderate diastolic dysfunction can manage the condition and reduce the risk of complications such as heart failure. Early diagnosis, personalized treatment plans, and ongoing monitoring are key to effectively managing this condition and preventing it from progressing to more severe stages.
Related topics: