Mitral valve failure, also known as mitral valve insufficiency or mitral regurgitation, is a significant cardiovascular condition that impacts the mitral valve’s ability to regulate blood flow within the heart. The mitral valve, located between the left atrium and left ventricle, plays a crucial role in ensuring that blood flows in one direction—from the atrium to the ventricle. When this valve fails to close properly, blood can leak backward (regurgitate) into the left atrium, causing a variety of complications.
Mitral valve failure can range from mild to severe, and if left untreated, it can lead to more serious heart conditions such as heart failure, atrial fibrillation, or even endocarditis. The condition often requires prompt diagnosis and, depending on severity, may involve medical management or surgical intervention. This article will explore the causes, symptoms, and treatments of mitral valve failure in detail to provide a comprehensive understanding of this heart condition.
Causes of Mitral Valve Failure
Mitral valve failure can occur due to a variety of reasons, ranging from congenital defects to acquired heart conditions.
Understanding the underlying causes of mitral valve failure is crucial for determining the most appropriate treatment options. The causes can be classified into two main categories: primary and secondary.
Primary Causes
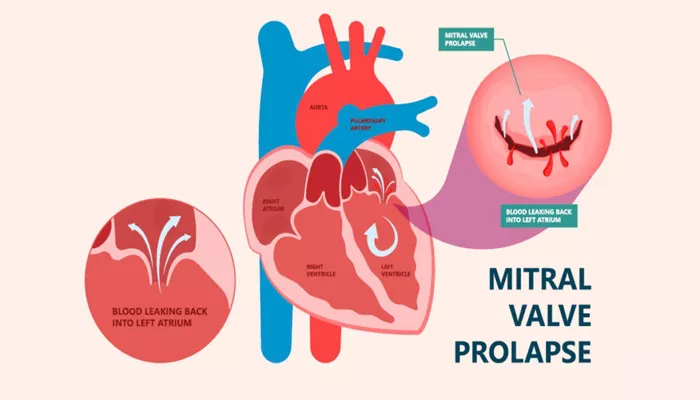
Mitral Valve Prolapse (MVP): Mitral valve prolapse is one of the most common causes of primary mitral regurgitation. In MVP, the mitral valve’s leaflets become enlarged or stretched and bulge back into the left atrium during contraction. This abnormality can prevent the valve from sealing tightly, leading to the backward flow of blood into the atrium. Although MVP can occur without symptoms, it can sometimes lead to progressive mitral regurgitation over time.
Rheumatic Heart Disease: Rheumatic fever, a complication of strep throat, can cause damage to the heart valves, including the mitral valve. Over time, this damage can result in scarring and deformity of the valve, leading to mitral regurgitation.
Rheumatic heart disease is still a leading cause of mitral valve failure in some parts of the world, especially in areas where access to antibiotics is limited.
Endocarditis: Endocarditis is an infection of the heart’s inner lining, including the heart valves. When the mitral valve is infected, it can lead to valve destruction, causing regurgitation. Endocarditis typically occurs in people with preexisting heart conditions, such as valvular disease or congenital heart defects.
Degenerative Valve Disease: As people age, the mitral valve’s structural integrity can deteriorate. The valve’s leaflets and supporting structures, such as the chordae tendineae (the cords that help hold the valve in place), may become weakened or damaged. This degeneration can result in mitral valve failure.
Secondary Causes
Coronary Artery Disease: Coronary artery disease (CAD) can indirectly contribute to mitral valve failure. A heart attack can damage the muscle around the mitral valve, causing it to lose its ability to function properly. This damage may also lead to dilation of the left ventricle, further impairing the valve’s ability to close completely.
Left Ventricular Dilation: In cases of heart failure or other forms of cardiomyopathy, the left ventricle may become dilated, which can distort the shape and function of the mitral valve. As the ventricle enlarges, the valve may no longer align correctly, resulting in regurgitation.
Hypertrophic Cardiomyopathy: Hypertrophic cardiomyopathy (HCM) is a condition where the heart muscle becomes abnormally thickened.
This can affect the mitral valve by preventing it from closing properly, which can lead to mitral regurgitation.
Congenital Heart Defects: Some individuals are born with abnormalities of the mitral valve that lead to improper function, such as a valve with too many or too few leaflets. These congenital defects can lead to early-onset mitral valve failure.
Symptoms of Mitral Valve Failure
The symptoms of mitral valve failure can vary significantly depending on the severity of the condition. Some individuals with mild mitral regurgitation may not experience noticeable symptoms, while others with severe regurgitation may experience a range of debilitating symptoms. Common symptoms include:
1. Shortness of Breath
As mitral valve failure progresses, blood may back up into the lungs, causing fluid accumulation and shortness of breath, especially during physical activity or when lying flat. This symptom is a common indicator of worsening mitral regurgitation and may signal the need for intervention.
2. Fatigue
Individuals with mitral valve failure often experience chronic fatigue due to reduced blood flow and decreased oxygen delivery to tissues.
This tiredness can affect daily activities and reduce overall quality of life.
3. Heart Palpitations
Mitral valve regurgitation can lead to an irregular heartbeat or arrhythmias, such as atrial fibrillation. This condition occurs when the left atrium is overfilled with blood, leading to increased pressure and changes in heart rhythm. People may experience palpitations or a sensation of the heart racing or skipping beats.
4. Chest Pain
Some individuals with mitral valve failure may experience chest pain or discomfort, especially if there is a related condition such as coronary artery disease or ischemia. However, chest pain is not as common in mitral regurgitation as it is in conditions like angina or heart attack.
5. Swelling in the Legs, Ankles, or Abdomen
As the condition progresses, the heart’s ability to pump blood effectively diminishes, which can lead to fluid buildup in the lower extremities (edema) or the abdomen. This swelling is a common symptom in heart failure.
6. Coughing or Wheezing
Fluid buildup in the lungs due to left-sided heart failure can lead to coughing or wheezing. This is a result of pulmonary congestion, where the blood returning to the heart backs up into the lungs, causing fluid leakage into lung tissue.
7. Syncope (Fainting)
In severe cases of mitral valve failure, individuals may experience fainting due to decreased blood flow to the brain. This occurs when the heart is unable to maintain an adequate cardiac output, especially during physical exertion.
Treatment of Mitral Valve Failure
The treatment for mitral valve failure depends on the severity of the condition and the presence of symptoms. Treatment options may include medications, lifestyle changes, or surgical interventions. The goal of treatment is to relieve symptoms, prevent complications, and improve the quality of life for the patient.
1. Medications
While medications cannot repair a damaged mitral valve, they can help manage symptoms and prevent further complications. Common medications used in the treatment of mitral valve failure include:
Diuretics: To reduce fluid buildup and relieve symptoms of congestion (e.g., swelling and shortness of breath).
Beta-Blockers: To slow the heart rate and prevent arrhythmias.
Angiotensin-Converting Enzyme (ACE) Inhibitors: To relax blood vessels and reduce the workload on the heart.
Aldosterone Antagonists: To reduce fluid retention and control high blood pressure.
Anticoagulants: To prevent blood clots, especially in patients with atrial fibrillation.
2. Surgical Treatment
In more severe cases of mitral valve failure, surgery may be required to repair or replace the mitral valve. The two primary surgical options are:
a. Mitral Valve Repair
When possible, mitral valve repair is preferred over replacement. This procedure involves reconstructing the existing valve to restore proper function. Mitral valve repair can involve techniques such as:
Chordal replacement or shortening: To fix the tendons that support the valve.
Annuloplasty: To tighten the ring surrounding the valve.
Leaflet repair: To reshape or reattach the valve leaflets.
b. Mitral Valve Replacement
In cases where repair is not feasible, the damaged mitral valve may need to be replaced with a mechanical or bioprosthetic valve. Mechanical valves are durable but require lifelong anticoagulation therapy, while bioprosthetic valves may wear out over time but do not require anticoagulants.
3. Minimally Invasive Surgery
For certain patients, minimally invasive procedures such as catheter-based repair or valve replacement may be appropriate.
These less invasive techniques involve smaller incisions and a faster recovery time compared to traditional open-heart surgery.
4. Lifestyle Modifications
In addition to medical and surgical treatments, lifestyle changes can play an important role in managing mitral valve failure. These may include:
Adopting a heart-healthy diet: Reducing salt intake, avoiding excess fats, and eating a balanced diet to support heart function.
Regular exercise: Maintaining physical activity as tolerated to strengthen the heart.
Managing weight and blood pressure: Keeping these factors under control can reduce the strain on the heart.
Conclusion
Mitral valve failure is a serious condition that can significantly impact heart function and overall health. While mild cases may be manageable with medication and monitoring, more severe cases often require surgical intervention to repair or replace the mitral valve. Early detection and timely treatment are essential to prevent complications such as heart failure or arrhythmias. If you suspect that you may have mitral valve failure, it is crucial to seek medical advice from a cardiologist for an accurate diagnosis and appropriate treatment plan.
Related topics: