In the intricate landscape of cardiovascular anatomy, the coronary arteries play a pivotal role in supplying oxygenated blood to the heart muscle. Among the terminologies frequently encountered in the realm of cardiology, “native coronary artery” stands out as a fundamental concept with profound clinical implications. This article aims to elucidate the intricacies surrounding native coronary arteries, exploring their anatomy, physiological function, and clinical significance in cardiovascular health and disease management.
Anatomy of Native Coronary Arteries
Native coronary arteries refer to the arteries that originate directly from the aorta and supply blood to the myocardium, or heart muscle. These arteries are distinct from graft arteries, such as those used in coronary artery bypass grafting (CABG) procedures, which are often harvested from elsewhere in the body and implanted to bypass diseased coronary arteries.
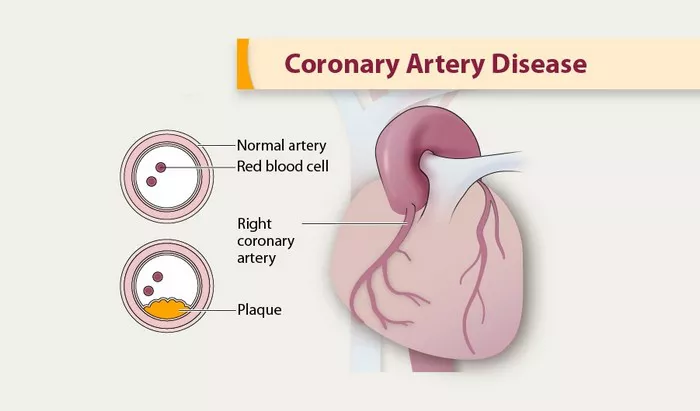
The native coronary artery system typically consists of two main arteries: the left main coronary artery (LMCA) and the right coronary artery (RCA). The LMCA further branches into the left anterior descending artery (LAD) and the left circumflex artery (LCx). The LAD supplies blood to the anterior portion of the heart, while the LCx nourishes the lateral wall. The RCA, on the other hand, primarily serves the posterior and inferior aspects of the heart.
The anatomy of native coronary arteries is subject to considerable variation among individuals. An understanding of this variability is crucial for diagnostic and interventional procedures in cardiology. Variations may include differences in the origin, course, and branching patterns of these arteries, which can influence the management of coronary artery disease (CAD) and other cardiac conditions.
Physiological Function of Native Coronary Arteries
The primary function of native coronary arteries is to deliver oxygenated blood to the myocardium, ensuring its metabolic needs are met for optimal cardiac function. During systole, when the heart contracts, coronary arteries experience decreased blood flow due to compression. Conversely, during diastole, when the heart relaxes and fills with blood, coronary perfusion increases, allowing for greater oxygen delivery to the myocardium.
The regulation of coronary blood flow is governed by a complex interplay of factors, including metabolic demands, neural inputs, and local vasodilator and vasoconstrictor substances. Endothelial cells lining the coronary arteries play a crucial role in mediating these processes by releasing vasodilators such as nitric oxide in response to various stimuli, including shear stress and metabolic factors.
Disturbances in coronary blood flow regulation can lead to myocardial ischemia, a condition characterized by inadequate oxygen supply to the heart muscle. Chronic ischemia may contribute to the development of CAD, whereas acute ischemia can precipitate myocardial infarction (MI) or heart attack, which constitutes a medical emergency requiring prompt intervention.
Clinical Significance of Native Coronary Arteries
Native coronary arteries are central to the pathophysiology and management of various cardiovascular disorders, including CAD, MI, and heart failure. Understanding the clinical significance of these arteries is essential for risk stratification, diagnosis, and treatment planning in patients with cardiac conditions.
CAD, the leading cause of morbidity and mortality worldwide, results from the accumulation of atherosclerotic plaque within the coronary arteries, leading to luminal narrowing or obstruction. The extent and severity of CAD, as assessed by imaging modalities such as coronary angiography or computed tomography angiography (CTA), influence treatment decisions, including medical therapy, percutaneous coronary intervention (PCI), or surgical revascularization with CABG.
The identification of significant stenoses or blockages in native coronary arteries guides the selection of revascularization strategies aimed at restoring blood flow to ischemic myocardial territories. In PCI, a catheter-based procedure, stents may be deployed to scaffold the narrowed segment of the artery and restore luminal patency. Alternatively, CABG involves surgical grafting of bypass conduits, such as the internal mammary artery or saphenous vein, to bypass obstructed coronary segments, thereby augmenting myocardial perfusion.
In addition to CAD, native coronary arteries are implicated in the pathogenesis of acute coronary syndromes (ACS), encompassing unstable angina, non-ST-segment elevation MI (NSTEMI), and ST-segment elevation MI (STEMI). These conditions result from the rupture or erosion of atherosclerotic plaque, leading to thrombus formation and acute arterial occlusion. Timely reperfusion therapy, achieved through PCI or thrombolytic therapy, is paramount in salvaging jeopardized myocardium and minimizing myocardial injury in patients presenting with ACS.
Furthermore, native coronary arteries play a crucial role in the assessment of myocardial viability and contractile reserve in patients with heart failure. Ischemic cardiomyopathy, characterized by impaired myocardial function secondary to CAD, necessitates the evaluation of viable myocardium amenable to revascularization. Imaging techniques such as stress echocardiography, myocardial perfusion imaging, and cardiac magnetic resonance imaging (MRI) facilitate the identification of viable myocardium and inform therapeutic decision-making in this patient population.
Conclusion
Native coronary arteries represent the lifeline of the myocardium, ensuring adequate oxygen supply to sustain cardiac function. A thorough understanding of their anatomy, physiological function, and clinical significance is imperative for healthcare professionals involved in the management of cardiovascular disease. By elucidating the complexities surrounding native coronary arteries, this article aims to empower clinicians with the knowledge necessary to optimize patient care and outcomes in the realm of cardiovascular medicine.