Coronary arteriosclerosis in native arteries is a complex medical condition that affects millions of individuals worldwide. As one of the leading causes of cardiovascular disease, understanding its mechanisms, risk factors, diagnosis, and management is crucial for healthcare professionals and patients alike. This comprehensive article aims to delve into the intricacies of coronary arteriosclerosis in native arteries, shedding light on its pathophysiology, clinical manifestations, diagnostic modalities, treatment options, and preventive strategies.
Pathophysiology
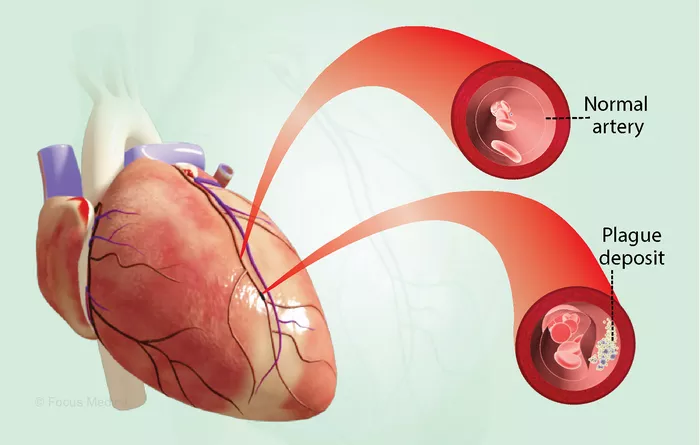
Coronary arteriosclerosis, often interchangeably referred to as coronary artery disease (CAD), is characterized by the narrowing or blockage of coronary arteries due to the buildup of plaque within their walls. Plaque is composed of cholesterol, fatty substances, cellular waste products, calcium, and fibrin, which accumulate over time and form atherosclerotic lesions. These lesions can impede blood flow to the myocardium, leading to ischemia and potentially resulting in myocardial infarction (MI) or sudden cardiac death.
The process of arteriosclerosis begins with endothelial injury, triggered by various risk factors such as hypertension, hyperlipidemia, smoking, diabetes mellitus, and inflammation. Endothelial dysfunction allows low-density lipoprotein (LDL) cholesterol to infiltrate the arterial wall, where it undergoes oxidative modification and becomes atherogenic. Monocytes adhere to the dysfunctional endothelium and migrate into the subendothelial space, where they differentiate into macrophages and engulf oxidized LDL particles, forming foam cells. This initiates an inflammatory response, attracting more immune cells and promoting the release of cytokines and growth factors, further exacerbating plaque formation.
As the atherosclerotic plaque progresses, it undergoes remodeling, with the fibrous cap becoming increasingly vulnerable to rupture. Plaque rupture exposes thrombogenic material to the bloodstream, leading to platelet aggregation, thrombus formation, and acute coronary syndromes (ACS). Alternatively, gradual plaque growth may result in luminal stenosis, limiting coronary blood flow and causing angina pectoris upon exertion.
Clinical Manifestations
The clinical presentation of coronary arteriosclerosis varies widely depending on the severity and location of arterial stenosis, as well as individual patient characteristics. Common symptoms include chest pain or discomfort (angina), dyspnea, fatigue, palpitations, and diaphoresis. Angina typically manifests as a tightness, pressure, squeezing, or burning sensation in the chest, often precipitated by physical exertion or emotional stress and relieved by rest or nitroglycerin.
In some cases, coronary arteriosclerosis may be asymptomatic, especially in its early stages. However, silent ischemia can still lead to myocardial injury and contribute to the progression of CAD. Additionally, certain patient populations, such as those with diabetes mellitus or advanced age, may exhibit atypical symptoms or present with complications such as heart failure or arrhythmias.
Diagnosis
The diagnosis of coronary arteriosclerosis involves a combination of clinical assessment, non-invasive testing, and invasive procedures. A thorough medical history and physical examination provide valuable insights into the patient’s risk factors, symptomatology, and overall cardiovascular health. Laboratory investigations, including lipid profile, fasting glucose, and cardiac biomarkers (e.g., troponin), aid in risk stratification and identifying comorbid conditions.
Non-invasive imaging modalities such as electrocardiography (ECG), stress testing, echocardiography, and cardiac computed tomography (CT) angiography can help evaluate myocardial ischemia, assess ventricular function, and visualize coronary anatomy. Stress testing, whether performed with exercise or pharmacological agents, induces myocardial demand ischemia and allows for the detection of reversible perfusion defects indicative of CAD.
When non-invasive testing is inconclusive or suggestive of significant coronary artery disease, invasive coronary angiography remains the gold standard for definitive diagnosis and treatment planning. This procedure involves the selective injection of radiographic contrast into the coronary arteries, enabling visualization of luminal narrowing, plaque morphology, and the presence of obstructive lesions. Fractional flow reserve (FFR) and intravascular ultrasound (IVUS) provide additional information regarding lesion severity and vessel characteristics, guiding decisions regarding revascularization.
Treatment Options
The management of coronary arteriosclerosis aims to alleviate symptoms, improve prognosis, and reduce the risk of cardiovascular events through lifestyle modifications, pharmacotherapy, and revascularization procedures. Lifestyle interventions, including smoking cessation, regular exercise, a heart-healthy diet, weight management, and stress reduction, form the cornerstone of primary and secondary prevention efforts. These measures address modifiable risk factors and promote cardiovascular health across the lifespan.
Pharmacotherapy plays a crucial role in the medical management of coronary arteriosclerosis, targeting various aspects of the underlying pathophysiology. Antiplatelet agents such as aspirin and P2Y12 inhibitors reduce the risk of thrombotic events by inhibiting platelet activation and aggregation. Statins, along with other lipid-lowering agents such as ezetimibe and PCSK9 inhibitors, lower LDL cholesterol levels and stabilize atherosclerotic plaques, thereby mitigating disease progression.
In addition to antiplatelet and lipid-lowering therapy, patients with symptomatic CAD may require antianginal medications to alleviate chest pain and improve exercise tolerance. Beta-blockers, calcium channel blockers, nitrates, and ranolazine are commonly used to reduce myocardial oxygen demand, increase coronary blood flow, and alleviate angina symptoms. Furthermore, medications targeting hypertension, diabetes mellitus, and other comorbidities are essential for optimizing cardiovascular risk factor control and preventing disease exacerbation.
Revascularization procedures, including percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), are indicated for patients with significant coronary artery stenosis who remain symptomatic despite optimal medical therapy or those at high risk of adverse cardiovascular events. PCI involves the deployment of stents to restore blood flow through the occluded or narrowed coronary artery, whereas CABG utilizes autologous or synthetic conduits to bypass obstructed segments of the coronary circulation. The choice between PCI and CABG depends on the extent and complexity of coronary disease, as well as patient-specific factors such as comorbidities, anatomy, and preferences.
Preventive Strategies
Preventing coronary arteriosclerosis and its complications requires a multifaceted approach addressing both individual and population-level factors. Public health initiatives aimed at promoting healthy behaviors, reducing tobacco use, improving dietary habits, and increasing physical activity can have a significant impact on cardiovascular risk reduction at the societal level. Government policies, healthcare regulations, and community interventions play crucial roles in creating environments conducive to cardiovascular health and facilitating access to preventive services.
At the individual level, primary prevention efforts focus on identifying and modifying risk factors before the onset of symptomatic disease. Risk assessment tools such as the Framingham Risk Score, American College of Cardiology/American Heart Association (ACC/AHA) ASCVD Risk Estimator, and QRISK provide valuable information regarding an individual’s 10-year risk of developing cardiovascular events, guiding risk stratification and preventive interventions. Targeting modifiable risk factors such as hypertension, dyslipidemia, diabetes mellitus, obesity, and sedentary lifestyle through lifestyle modifications and pharmacotherapy can significantly reduce the burden of coronary arteriosclerosis and its sequelae.
Furthermore, secondary prevention strategies aim to mitigate the risk of recurrent cardiovascular events in patients with established CAD. Intensive risk factor management, including aggressive lipid-lowering therapy, blood pressure control, glycemic optimization, smoking cessation, and adherence to cardioprotective medications, is paramount in reducing morbidity and mortality in this population. Cardiac rehabilitation programs offer structured exercise training, risk factor education, psychosocial support, and secondary prevention counseling to patients recovering from acute coronary events, empowering them to adopt healthier lifestyles and adhere to prescribed therapies.
Conclusion
Coronary arteriosclerosis in native arteries represents a significant public health challenge worldwide, contributing to substantial morbidity, mortality, and healthcare expenditures. Understanding the pathophysiology, clinical manifestations, diagnostic approaches, treatment modalities, and preventive strategies associated with CAD is essential for healthcare professionals involved in the care of patients with cardiovascular disease. By addressing modifiable risk factors, optimizing medical therapy, and promoting healthy lifestyles, individuals and communities can work together to reduce the burden of coronary arteriosclerosis and improve cardiovascular outcomes for all.