Spontaneous coronary artery dissection (SCAD) is a rare but potentially life-threatening condition that occurs when a tear forms in one of the coronary arteries, leading to separation of the layers of the artery wall and potential obstruction of blood flow to the heart muscle. Once considered a rare phenomenon primarily observed in young, healthy females, SCAD is increasingly recognized as a cause of acute coronary syndrome (ACS) across diverse demographic groups. Despite advancements in medical imaging and clinical awareness, the etiology and pathophysiology of SCAD remain poorly understood, posing challenges for accurate diagnosis and management. This article aims to explore the current understanding of SCAD, including its epidemiology, risk factors, clinical presentation, diagnostic modalities, and management strategies, with a focus on unraveling the enigmatic mechanisms underlying this intriguing condition.
Epidemiology and Clinical Presentation
Although SCAD was historically considered a rare occurrence, recent studies suggest that it may account for up to 4% of cases of ACS. The incidence of SCAD varies across different populations, with a predilection for younger individuals, particularly females. Women comprise approximately 90% of SCAD cases, with a mean age of onset typically in the fourth to fifth decade of life. Notably, SCAD is increasingly recognized as a cause of ACS in males and older individuals, challenging previous perceptions of its demographic distribution.
The clinical presentation of SCAD can vary widely, ranging from asymptomatic cases incidentally detected on imaging studies to life-threatening myocardial infarction (MI) or sudden cardiac death. Common symptoms of SCAD-related ACS include chest pain or discomfort, dyspnea, palpitations, and syncope, which can mimic other cardiac conditions such as atherosclerotic coronary artery disease. The variability in clinical presentation underscores the importance of maintaining a high index of suspicion for SCAD, particularly in young individuals and females presenting with ACS in the absence of traditional cardiovascular risk factors.
Risk Factors and Predisposing Conditions
Identifying the risk factors and predisposing conditions associated with SCAD is crucial for understanding its pathogenesis and guiding clinical management. While the precise mechanisms underlying SCAD remain incompletely understood, several factors have been implicated in its development, including:
1. Female Gender: Women are disproportionately affected by SCAD, with hormonal and reproductive factors potentially playing a role in its pathogenesis. The majority of SCAD cases occur in women during the peripartum period or in association with hormonal changes such as pregnancy, oral contraceptive use, or hormone replacement therapy.
2. Fibromuscular Dysplasia (FMD): FMD, a non-inflammatory arteriopathy characterized by abnormal growth and development of arterial walls, is strongly associated with SCAD. Up to 70% of individuals with SCAD have evidence of FMD, suggesting a potential common underlying pathophysiology.
3. Genetic Predisposition: Emerging evidence suggests a genetic component to SCAD susceptibility, with familial clustering and genetic variants implicated in arterial wall integrity, collagen synthesis, and extracellular matrix remodeling. Genome-wide association studies have identified potential susceptibility loci associated with SCAD, although further research is needed to elucidate the specific genetic determinants.
4. Connective Tissue Disorders: Certain connective tissue disorders, such as Ehlers-Danlos syndrome, Marfan syndrome, and Loeys-Dietz syndrome, are associated with structural abnormalities in arterial walls and an increased risk of arterial dissections, including SCAD.
5. Physical Stressors: Intense physical exertion, such as extreme exercise or weightlifting, has been implicated as a trigger for SCAD, particularly in individuals with underlying arterial fragility or predisposing conditions.
6. Emotional Stress and Vasoconstrictive Substances: Emotional stressors and vasoconstrictive substances, such as cocaine or sympathomimetic agents, may precipitate SCAD through mechanisms involving coronary artery spasm and endothelial dysfunction.
Pathophysiology of Spontaneous Coronary Artery Dissection
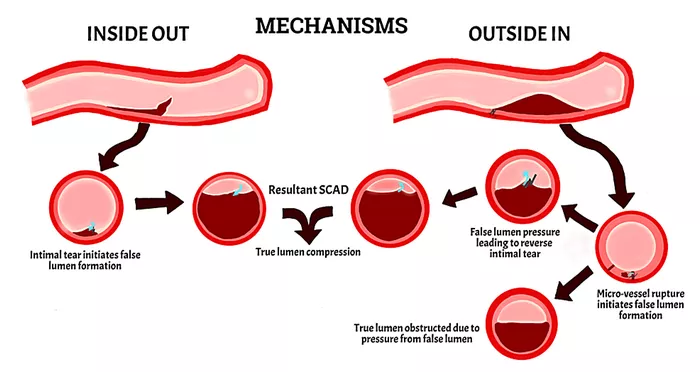
The pathophysiology of SCAD involves a complex interplay of mechanical, hemodynamic, and biological factors that culminate in the development of arterial wall injury and dissection. While the exact sequence of events leading to SCAD remains elusive, several proposed mechanisms have been postulated:
1. Arterial Wall Vulnerability: Structural abnormalities in the arterial wall, including medial degeneration, fibromuscular dysplasia, and connective tissue disorders, render the coronary arteries susceptible to mechanical stress and injury. Histopathological studies of SCAD lesions demonstrate disruption of the arterial media, with evidence of smooth muscle cell proliferation, elastin degradation, and collagen disorganization.
2. Shear Forces and Hemodynamic Stress: Hemodynamic forces exerted on the coronary arteries during systole and diastole may contribute to the initiation and propagation of arterial dissection. Shear forces generated by alterations in blood flow patterns, endothelial dysfunction, and turbulence at branch points or areas of arterial curvature may predispose to intimal tears and intramural hematoma formation.
3. Endothelial Dysfunction and Inflammation: Endothelial dysfunction, characterized by impaired vasodilation, increased vascular permeability, and proinflammatory cytokine release, has been implicated in the pathogenesis of SCAD. Disruption of the endothelial barrier function may facilitate the transmigration of inflammatory cells into the arterial wall, promoting oxidative stress, matrix metalloproteinase activation, and extracellular matrix remodeling.
4. Hormonal and Reproductive Factors: Hormonal fluctuations associated with pregnancy, menstruation, or exogenous hormone use may contribute to arterial wall fragility and susceptibility to SCAD. Estrogen and progesterone receptors expressed in the arterial wall regulate vascular tone, smooth muscle cell proliferation, and extracellular matrix synthesis, suggesting a potential role in SCAD pathophysiology.
5. Genetic and Familial Factors: Genetic predisposition and familial clustering of SCAD cases suggest a hereditary component to its pathogenesis. Mutations in genes encoding proteins involved in arterial wall integrity, collagen synthesis, and extracellular matrix remodeling may disrupt the structural and functional integrity of the coronary arteries, predisposing to spontaneous dissection.
Diagnostic Evaluation and Imaging Modalities
Accurate diagnosis of SCAD relies on a combination of clinical suspicion, electrocardiographic findings, biomarker analysis, and multimodal imaging studies. Electrocardiography (ECG) may demonstrate ST-segment elevation or depression, T-wave inversion, or other ischemic changes consistent with ACS. Biomarkers such as troponin and creatine kinase-MB (CK-MB) are commonly elevated in SCAD-related ACS, reflecting myocardial injury secondary to coronary artery obstruction.
Multimodal imaging modalities play a central role in the diagnosis and characterization of SCAD lesions, including:
1. Coronary Angiography: Invasive coronary angiography remains the gold standard for diagnosing SCAD, allowing direct visualization of the coronary arteries and identification of characteristic angiographic features such as multiple radiolucent lumens, contrast staining, and arterial dissection flaps. However, conventional angiography may underestimate the extent of arterial involvement and fail to delineate the true lumen in cases of intramural hematoma or extracoronary extension.
2. Intravascular Imaging: Intravascular imaging techniques such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT) provide high-resolution imaging of the coronary artery wall and lumen, enabling precise assessment of plaque morphology, intramural hematoma, and dissection flap. IVUS and OCT can differentiate between true and false lumens, assess the extent of arterial wall involvement, and guide percutaneous interventions such as stent placement or balloon angioplasty.
3. Cardiac Magnetic Resonance Imaging (MRI): Cardiac MRI is a non-invasive imaging modality that offers multiplanar visualization of the heart and coronary arteries, with superior soft tissue contrast and spatial resolution compared to conventional angiography. Cardiac MRI can accurately depict the presence and extent of intramural hematoma, myocardial ischemia, and myocardial infarction in patients with SCAD, aiding in risk stratification and prognostication.
4. Computed Tomography Angiography (CTA): Coronary CTA is a non-invasive imaging technique that provides three-dimensional reconstruction of the coronary arteries and detection of luminal narrowing, dissection, or intramural hematoma. Coronary CTA is particularly useful in hemodynamically stable patients with suspected SCAD, offering rapid and comprehensive evaluation of the coronary anatomy without the need for invasive catheterization.
Management Strategies and Therapeutic Considerations
The management of SCAD remains challenging due to its diverse clinical presentation, variable natural history, and limited evidence-based guidelines. Treatment strategies for SCAD are largely based on expert consensus and clinical experience, with an emphasis on individualized risk assessment and multidisciplinary care. Key considerations in the management of SCAD include:
1. Conservative Management: Conservative management with medical therapy alone may be appropriate for hemodynamically stable patients with non-obstructive SCAD and minimal myocardial ischemia. Medical therapy typically includes antiplatelet agents such as aspirin and P2Y12 inhibitors (e.g., clopidogrel), beta-blockers or calcium channel blockers for symptom control, and statins for secondary prevention of atherosclerosis.
2. Percutaneous Coronary Intervention (PCI): In patients with hemodynamically significant SCAD and evidence of ongoing myocardial ischemia, PCI may be indicated to restore coronary blood flow and relieve myocardial ischemia. However, PCI in SCAD requires careful consideration of lesion morphology, location, and extent of arterial involvement to minimize the risk of iatrogenic complications such as propagation of dissection, stent malapposition, or coronary perforation.
3. Coronary Artery Bypass Grafting (CABG): CABG may be considered in select cases of SCAD with complex coronary anatomy, extensive arterial involvement, or recurrent ischemic events refractory to medical therapy or PCI. CABG offers the advantage of complete revascularization and long-term patency of bypass grafts, particularly in patients with multivessel SCAD or concomitant coronary artery disease.
4. Long-Term Follow-Up and Surveillance: Long-term follow-up and surveillance are essential for patients with SCAD to monitor for recurrent ischemic events, progression of arterial dissection, and development of coronary artery aneurysms or pseudoaneurysms. Serial clinical evaluations, electrocardiography, biomarker analysis, and imaging studies such as coronary angiography or cardiac MRI may be performed to assess treatment response and guide ongoing management.
Future Directions and Research Opportunities
Despite significant advances in the understanding and management of SCAD, many questions remain unanswered regarding its etiology, risk stratification, and optimal treatment strategies. Future research efforts should focus on elucidating the underlying mechanisms of SCAD, identifying novel biomarkers and imaging modalities for early detection and risk prediction, and conducting prospective studies to evaluate the efficacy of different treatment approaches. Collaborative multicenter registries and clinical trials are needed to standardize diagnostic criteria, establish evidence-based guidelines, and improve outcomes for patients with this enigmatic condition.
Conclusion
Spontaneous coronary artery dissection is a rare but increasingly recognized cause of acute coronary syndrome, particularly in young individuals and females without traditional cardiovascular risk factors. The pathophysiology of SCAD involves a complex interplay of mechanical, hemodynamic, and biological factors, with genetic predisposition, arterial wall vulnerability, and hormonal influences contributing to its development. Accurate diagnosis and management of SCAD require a multidisciplinary approach, incorporating clinical suspicion, electrocardiographic findings, biomarker analysis, and multimodal imaging studies. Although the optimal treatment strategies for SCAD remain uncertain, conservative management with medical therapy alone or invasive interventions such as PCI or CABG may be considered based on individual patient characteristics and clinical presentation. Further research is needed to advance our understanding of SCAD pathogenesis, refine diagnostic algorithms, and optimize treatment outcomes for this intriguing and challenging condition.