Heart failure remains a critical global health concern, affecting millions of individuals annually. It manifests in various forms, with left and right heart failure being two primary classifications. While they share similarities in symptomatology and treatment approaches, understanding their unique pathophysiology and clinical presentations is crucial for accurate diagnosis and targeted management. This comprehensive article delves into the intricate differences between left and right heart failure, providing clinicians and healthcare professionals with a comprehensive understanding of these conditions.
Overview
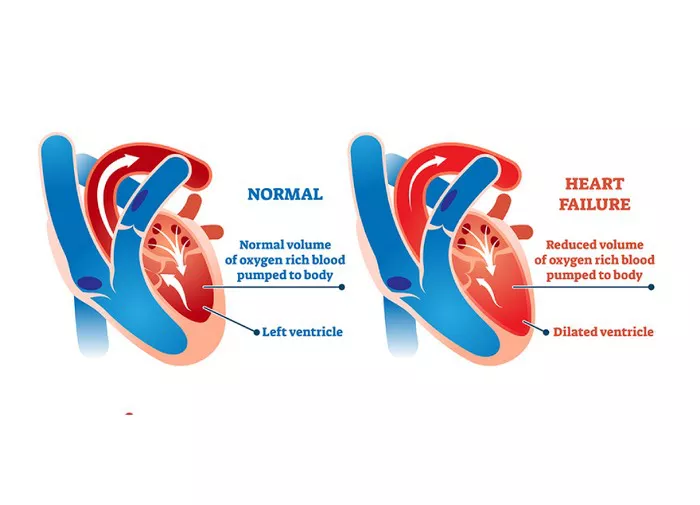
Heart failure is a complex clinical syndrome characterized by the heart’s inability to pump blood efficiently to meet the body’s metabolic demands. It results from structural or functional abnormalities impairing ventricular filling or ejection of blood. Left and right heart failure represent distinct subsets of this syndrome, each stemming from specific cardiac dysfunctions. While they often coexist, discerning their individual contributions is pivotal for effective management.
Anatomy and Physiology of the Heart
Before delving into the nuances of left and right heart failure, it is essential to review the basic anatomy and physiology of the heart. The heart comprises four chambers: two atria and two ventricles. The right atrium receives deoxygenated blood from the body via the superior and inferior vena cavae and pumps it into the right ventricle. The right ventricle then pumps this blood into the pulmonary circulation for oxygenation. Oxygenated blood returns to the left atrium from the lungs via the pulmonary veins and is pumped into the left ventricle. The left ventricle, being more muscular, generates the force necessary to propel oxygen-rich blood throughout the systemic circulation.
Left Heart Failure: Pathophysiology and Clinical Features
Left heart failure occurs when the left ventricle fails to pump blood adequately, leading to impaired systemic perfusion. It commonly results from chronic hypertension, coronary artery disease, or valvular heart disease. As the left ventricle weakens, blood accumulates in the pulmonary circulation, causing pulmonary congestion and edema. The hallmark symptom of left heart failure is dyspnea on exertion, which progresses to orthopnea and paroxysmal nocturnal dyspnea as the disease advances. Patients may also present with fatigue, cough, and fluid retention manifesting as peripheral edema.
Right Heart Failure: Pathophysiology and Clinical Features
Conversely, right heart failure occurs when the right ventricle fails to pump blood effectively into the pulmonary circulation. It often develops secondary to left heart failure, pulmonary hypertension, or chronic lung diseases such as chronic obstructive pulmonary disease (COPD). In right heart failure, systemic venous pressure increases, leading to jugular venous distention, hepatomegaly, and peripheral edema. Patients may experience fatigue, abdominal discomfort, and fluid retention, particularly in the lower extremities.
Etiology and Risk Factors
The etiology of left and right heart failure overlaps in several aspects, including coronary artery disease, hypertension, and valvular heart disease. However, certain risk factors may predispose individuals to one type of heart failure over the other. Left heart failure commonly arises from conditions associated with increased left ventricular afterload, such as systemic hypertension and aortic stenosis. On the other hand, right heart failure often ensues from pulmonary conditions causing elevated pulmonary vascular resistance, such as pulmonary hypertension and chronic lung diseases.
Diagnostic Evaluation
Accurate diagnosis of left and right heart failure relies on a comprehensive clinical assessment supplemented by various diagnostic modalities. History-taking and physical examination provide valuable insights into symptomatology and hemodynamic status. Laboratory tests, including brain natriuretic peptide (BNP) and cardiac troponins, aid in risk stratification and identifying underlying etiologies. Imaging studies such as echocardiography, cardiac MRI, and nuclear imaging offer detailed assessments of cardiac structure and function, facilitating differential diagnosis and treatment planning.
Treatment Strategies
Management of heart failure aims to alleviate symptoms, improve quality of life, and reduce morbidity and mortality. While treatment strategies for left and right heart failure share common principles, some interventions target specific pathophysiological mechanisms.
Left Heart Failure:
1. Pharmacotherapy: Angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), beta-blockers, and mineralocorticoid receptor antagonists (MRAs) constitute the cornerstone of medical therapy for left heart failure. They attenuate neurohormonal activation, reduce ventricular remodeling, and improve cardiac function.
2. Device Therapy: Cardiac resynchronization therapy (CRT) and implantable cardioverter-defibrillators (ICDs) are indicated in selected patients with left heart failure to optimize ventricular synchrony and prevent sudden cardiac death.
3. Revascularization: Coronary revascularization procedures, such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), may benefit patients with left heart failure secondary to ischemic heart disease.
Right Heart Failure:
1. Pulmonary Vasodilators: In patients with right heart failure secondary to pulmonary hypertension, pulmonary vasodilator therapy, including phosphodiesterase-5 inhibitors (e.g., sildenafil), endothelin receptor antagonists (e.g., bosentan), and prostacyclin analogs (e.g., epoprostenol), can improve pulmonary hemodynamics and exercise capacity.
2. Oxygen Therapy: Supplemental oxygen therapy is indicated in patients with chronic hypoxemia to alleviate pulmonary vasoconstriction and improve oxygen delivery to peripheral tissues.
3. Diuretics: Diuretics play a crucial role in managing fluid overload and relieving symptoms of congestion in right heart failure. Loop diuretics such as furosemide are commonly used to reduce systemic and pulmonary congestion.
Prognosis and Complications
Despite advances in heart failure management, the prognosis remains guarded, with high rates of morbidity and mortality. Left heart failure carries a worse prognosis compared to right heart failure, primarily due to its association with adverse cardiovascular events such as myocardial infarction and sudden cardiac death. However, right heart failure can progress rapidly in the setting of severe pulmonary hypertension or acute exacerbations of chronic lung disease, leading to hemodynamic instability and multiorgan dysfunction.
Conclusion
In conclusion, left and right heart failure represent distinct clinical entities with unique pathophysiological mechanisms and manifestations. While they often coexist and share common risk factors, recognizing their differences is paramount for accurate diagnosis and tailored management. A multidisciplinary approach involving healthcare professionals from cardiology, pulmonology, and primary care is essential to optimize outcomes and improve the quality of life for patients living with heart failure. Ongoing research and innovation in diagnostics and therapeutics promise to further enhance our understanding and management of these challenging conditions.