Hyperlipidemia, a condition characterized by elevated levels of lipids (fats) in the bloodstream, is a significant risk factor for cardiovascular diseases such as coronary artery disease, stroke, and peripheral artery disease. It poses a considerable public health concern globally, contributing to morbidity and mortality rates. While hyperlipidemia often manifests as high levels of cholesterol, particularly low-density lipoprotein (LDL) cholesterol, it encompasses a spectrum of lipid abnormalities. Understanding the multifaceted causes of hyperlipidemia is crucial for effective prevention, diagnosis, and management strategies.
Defining Hyperlipidemia
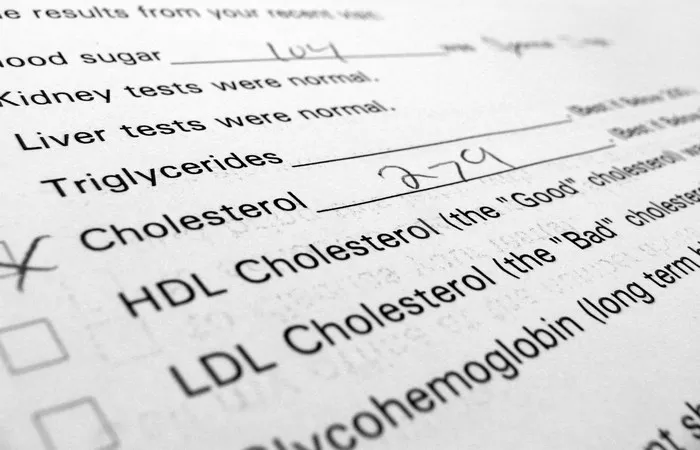
Hyperlipidemia refers to elevated concentrations of lipids in the blood, including cholesterol and triglycerides. These lipids circulate in the bloodstream within lipoprotein particles, which are classified based on their density: high-density lipoprotein (HDL), LDL, very-low-density lipoprotein (VLDL), and chylomicrons. While cholesterol is essential for various physiological processes, excessive levels, particularly LDL cholesterol, contribute to atherosclerosis and cardiovascular diseases (CVDs).
Genetic Predisposition: Familial Hyperlipidemias
One of the primary causes of hyperlipidemia is genetic predisposition. Familial hyperlipidemias are inherited disorders characterized by abnormal lipid metabolism, leading to elevated lipid levels from an early age. These disorders result from mutations in genes encoding proteins involved in lipid transport, metabolism, or regulation. Familial hyperlipidemias include familial hypercholesterolemia (FH), familial combined hyperlipidemia (FCHL), familial dysbetalipoproteinemia, and familial hypertriglyceridemia.
Lifestyle Factors: Dietary Habits and Physical Activity
Dietary habits and lifestyle choices significantly influence lipid levels and play a pivotal role in the development of hyperlipidemia. Consuming a diet high in saturated fats, trans fats, and cholesterol increases LDL cholesterol levels, while inadequate intake of fruits, vegetables, and fiber may exacerbate dyslipidemia. Moreover, excessive alcohol consumption can elevate triglyceride levels. Sedentary lifestyle and lack of physical activity contribute to obesity, insulin resistance, and dyslipidemia, further predisposing individuals to CVDs.
Metabolic Disorders: Insulin Resistance and Metabolic Syndrome
Insulin resistance, a hallmark of type 2 diabetes mellitus (T2DM), is closely intertwined with dyslipidemia. Insulin resistance impairs the ability of cells to respond to insulin, leading to compensatory hyperinsulinemia and dysregulation of lipid metabolism. Elevated insulin levels stimulate hepatic synthesis of VLDL cholesterol and inhibit lipolysis, promoting hypertriglyceridemia. Metabolic syndrome, characterized by a cluster of metabolic abnormalities including central obesity, dyslipidemia, hypertension, and insulin resistance, significantly increases the risk of CVDs.
Endocrine Disorders: Thyroid Dysfunction and Cushing’s Syndrome
Endocrine disorders can disrupt lipid metabolism and contribute to hyperlipidemia. Hypothyroidism, characterized by decreased thyroid hormone production, leads to elevated levels of LDL cholesterol and triglycerides due to reduced clearance of lipoproteins. Conversely, hyperthyroidism accelerates lipid metabolism, causing increased synthesis and turnover of lipids. Cushing’s syndrome, a condition characterized by excess cortisol production, promotes central obesity, insulin resistance, and dyslipidemia, predisposing individuals to CVDs.
Medications and Therapies: Pharmacological Inducers of Hyperlipidemia
Several medications and therapeutic interventions have been associated with dyslipidemia as a side effect. Certain classes of drugs, such as corticosteroids, antipsychotics, immunosuppressants, and diuretics, can adversely affect lipid metabolism and lead to hyperlipidemia. Moreover, hormonal therapies, including oral contraceptives and hormone replacement therapy, may alter lipid profiles in susceptible individuals. Awareness of medication-induced hyperlipidemia is essential for healthcare professionals to mitigate associated risks and optimize patient care.
Secondary Causes: Underlying Medical Conditions
Hyperlipidemia can arise secondary to various underlying medical conditions, necessitating thorough evaluation and management of the underlying etiology. Chronic kidney disease (CKD) disrupts lipid metabolism and clearance, leading to dyslipidemia and increased cardiovascular risk. Liver diseases, such as non-alcoholic fatty liver disease (NAFLD) and primary biliary cholangitis (PBC), can impair hepatic lipid metabolism and secretion, contributing to dyslipidemia. Additionally, certain inflammatory conditions, such as rheumatoid arthritis and systemic lupus erythematosus, are associated with dyslipidemia due to chronic inflammation and immune dysregulation.
Environmental Factors: Pollution and Toxins
Emerging evidence suggests that environmental factors, including air pollution and exposure to toxins, may impact lipid metabolism and contribute to the development of hyperlipidemia. Airborne pollutants, such as particulate matter (PM) and nitrogen oxides (NOx), have been linked to dyslipidemia, oxidative stress, and systemic inflammation, promoting atherosclerosis and CVDs. Furthermore, environmental toxins, such as persistent organic pollutants (POPs) and heavy metals, can disrupt lipid homeostasis and metabolic pathways, exacerbating dyslipidemia and metabolic disorders.
Conclusion
Hyperlipidemia is a multifactorial disorder influenced by genetic, lifestyle, metabolic, endocrine, medication-induced, secondary, and environmental factors. Comprehensive assessment of lipid profiles and identification of underlying causes are essential for guiding targeted interventions and reducing cardiovascular risk. Strategies aimed at promoting healthy lifestyle habits, managing comorbidities, optimizing medication regimens, and addressing environmental determinants are paramount in the prevention and management of hyperlipidemia. By elucidating the complex etiology of hyperlipidemia, healthcare professionals can implement personalized approaches to mitigate risk factors and improve patient outcomes in the era of precision medicine.