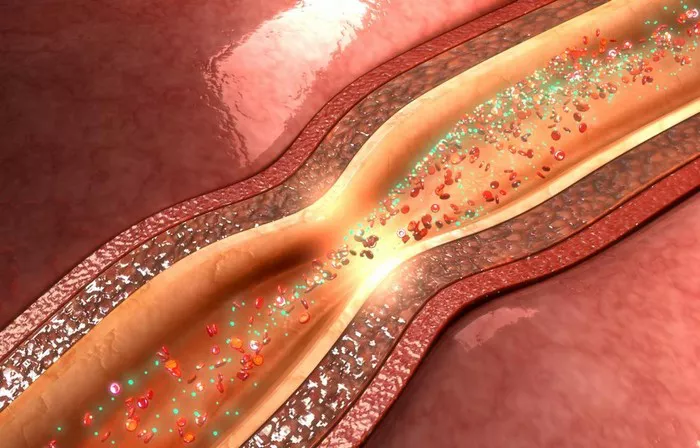
Vascular spasms, also known as vasospasms, are sudden contractions of the smooth muscle within the walls of blood vessels, leading to their constriction. These spasms can occur in arteries, veins, or capillaries, causing a range of symptoms from mild discomfort to severe complications such as ischemia or even tissue death. Understanding the triggers of vascular spasm is crucial for preventing and managing associated health risks. In this article, we delve into the various factors that can initiate vascular spasms and explore their implications for clinical practice and patient care.
Physiological Factors
1. Endothelial Dysfunction: The endothelium, a single layer of cells lining blood vessels, plays a pivotal role in regulating vascular tone and function. Dysfunction of the endothelium, often associated with conditions like atherosclerosis, hypertension, or diabetes, can disrupt the balance of vasoactive substances such as nitric oxide (NO) and endothelin, predisposing vessels to spasms.
2. Sympathetic Nervous System Activation: Stress, anxiety, and sympathetic stimulation can trigger the release of catecholamines such as adrenaline and noradrenaline. These neurotransmitters bind to adrenergic receptors on vascular smooth muscle cells, leading to their contraction and subsequent vasospasm.
3. Calcium Ion Imbalance: Intracellular calcium ions serve as crucial mediators of smooth muscle contraction. Abnormalities in calcium handling, such as excessive influx or impaired sequestration, can disrupt the physiological balance and promote sustained contraction of vascular smooth muscle, precipitating spasms.
4. Hormonal Influences: Hormones like serotonin, histamine, and thromboxane can exert vasoconstrictive effects, contributing to vascular spasms. Additionally, hormonal fluctuations associated with menstrual cycles or hormonal therapies may predispose certain individuals, particularly women, to vasospastic disorders such as Raynaud’s phenomenon.
Environmental Triggers
1. Cold Exposure: Exposure to cold temperatures can elicit peripheral vasoconstriction as part of the body’s thermoregulatory response. However, in susceptible individuals, particularly those with conditions like Raynaud’s disease, excessive or prolonged cold exposure may trigger exaggerated vascular spasms, leading to digital ischemia and tissue damage.
2. Chemical Irritants: Inhalation or exposure to chemical irritants, such as cigarette smoke, air pollutants, or certain industrial chemicals, can induce vascular smooth muscle contraction and inflammation, predisposing to vasospasm and endothelial injury.
3. Physical Trauma: Traumatic injury to blood vessels, either through external trauma or surgical interventions, can disrupt vascular integrity and trigger a cascade of inflammatory and vasoactive responses, culminating in vascular spasm and potential ischemic complications.
4. Mechanical Compression: Prolonged or repetitive mechanical compression of blood vessels, as seen in conditions like thoracic outlet syndrome or compartment syndrome, can impede blood flow and elicit vascular spasms, leading to tissue ischemia and neurovascular compromise.
Pathological Conditions
1. Atherosclerosis: Atherosclerotic plaques, characterized by the accumulation of cholesterol, inflammatory cells, and fibrous tissue within arterial walls, can narrow vessel lumens and disrupt endothelial function, promoting vascular spasm and thrombotic events.
2. Hypertension: Chronic elevation of blood pressure imposes increased mechanical stress on arterial walls, leading to vascular remodeling, endothelial dysfunction, and enhanced vasoconstrictor tone. These changes predispose hypertensive individuals to vascular spasms and end-organ damage.
3. Autoimmune Disorders: Systemic autoimmune conditions, such as systemic lupus erythematosus (SLE) or rheumatoid arthritis, can involve vascular inflammation and endothelial injury, increasing the susceptibility to vasospastic phenomena like vasculitis or Raynaud’s syndrome.
4. Hypercoagulable States: Disorders associated with increased blood clotting propensity, such as thrombophilia or disseminated intravascular coagulation (DIC), can promote microvascular thrombosis and endothelial dysfunction, exacerbating vascular spasm and ischemic complications.
Pharmacological Agents
1. Vasoactive Medications: Certain medications, including sympathomimetics, ergot alkaloids, or vasoconstrictor agents used in nasal decongestants or migraine treatments, can directly induce vascular smooth muscle contraction and trigger vasospastic episodes.
2. Chemotherapy Agents: Some chemotherapeutic drugs, such as cisplatin or vinca alkaloids, have been associated with peripheral neuropathy and vascular toxicity, potentially leading to vasospasm-related complications such as Raynaud’s phenomenon or digital ischemia.
3. Ergogenic Supplements: The use of ergogenic aids or performance-enhancing substances, such as anabolic steroids or amphetamines, can alter vascular tone and endothelial function, increasing the risk of vasospasm and cardiovascular events, particularly in susceptible individuals.
Psychosocial Factors
1. Stress and Anxiety: Psychological stressors, whether acute or chronic, can activate the sympathetic nervous system and trigger release of stress hormones, exacerbating vasoconstriction and promoting vascular spasms, especially in individuals with underlying cardiovascular risk factors.
2. Emotional Triggers: Emotional arousal or intense emotional experiences can elicit autonomic responses and sympathetic activation, leading to peripheral vasoconstriction and potential exacerbation of vasospastic disorders such as migraine headaches or Raynaud’s phenomenon.
Conclusion
Vascular spasms represent a complex interplay of physiological, environmental, pathological, pharmacological, and psychosocial factors, each contributing to the initiation and perpetuation of vascular smooth muscle contraction and endothelial dysfunction. Recognizing these triggers is paramount for clinicians in assessing individual risk profiles, implementing targeted preventive strategies, and optimizing management approaches for patients with vasospastic disorders. By addressing modifiable risk factors, promoting lifestyle modifications, and employing appropriate pharmacotherapy when indicated, healthcare providers can mitigate the impact of vascular spasms and improve patient outcomes in clinical practice.