Left heart failure is a complex condition that affects millions of people worldwide. It occurs when the left side of the heart is unable to pump blood effectively, leading to a range of symptoms and potential complications. While advances in medical science have improved outcomes for individuals with left heart failure, questions about life expectancy and prognosis remain common among patients and their families. In this article, we delve into the factors that influence life expectancy in left heart failure patients and discuss strategies for improving outcomes and quality of life.
Understanding Left Heart Failure
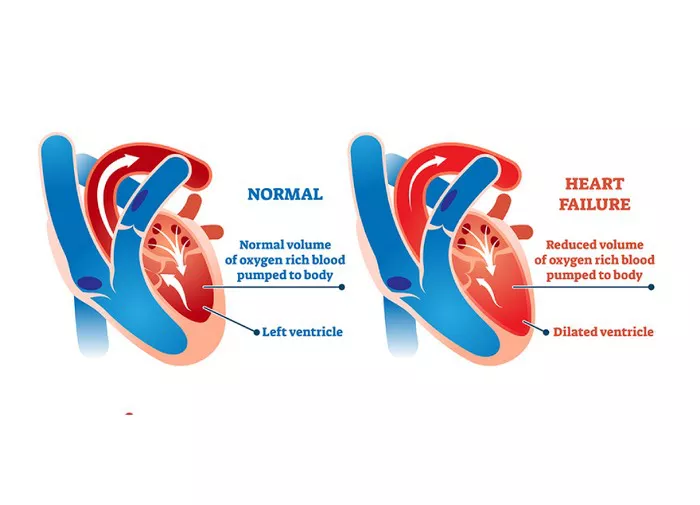
Before delving into life expectancy, it’s crucial to understand the basics of left heart failure. The heart has four chambers: two atria (upper chambers) and two ventricles (lower chambers). The left ventricle is responsible for pumping oxygen-rich blood from the lungs to the rest of the body. In left heart failure, the left ventricle becomes weak or stiff, impairing its ability to effectively pump blood.
Common causes of left heart failure include coronary artery disease, high blood pressure (hypertension), heart valve disease, and myocardial infarction (heart attack). These conditions can damage the heart muscle over time, leading to impaired function.
Prognostic Factors in Left Heart Failure
Several factors influence the prognosis of left heart failure patients. These factors can help healthcare providers and patients understand the likely course of the disease and make informed decisions about treatment and care.
1. Ejection Fraction (EF): The ejection fraction measures the percentage of blood that the left ventricle pumps out with each contraction. A normal EF is typically between 50% and 70%. In left heart failure, the EF may be reduced, indicating weakened heart function. A lower EF is associated with a poorer prognosis, although individual outcomes can vary widely.
2. Symptom Severity: The severity of symptoms such as shortness of breath (dyspnea), fatigue, and exercise intolerance can also impact prognosis. Patients with more severe symptoms may have a higher risk of complications and a poorer prognosis compared to those with milder symptoms.
3. Underlying Causes: The underlying cause of left heart failure can significantly influence prognosis. For example, heart failure due to coronary artery disease may have a different prognosis than heart failure caused by a heart valve disorder.
4. Coexisting Conditions: Patients with other health conditions such as diabetes, kidney disease, or lung disease may have a higher risk of complications and a poorer prognosis.
5. Treatment Response: How well a patient responds to treatment, including medications, lifestyle changes, and interventions like cardiac resynchronization therapy (CRT) or implantable cardioverter-defibrillators (ICDs), can also impact prognosis.
6. Age and Overall Health: Age and overall health status play a role in determining prognosis. Younger patients with fewer comorbidities may have better outcomes compared to older patients with multiple health issues.
7. Compliance with Treatment: Adherence to prescribed medications, dietary recommendations, and lifestyle modifications can influence long-term outcomes in left heart failure patients.
Life Expectancy in Left Heart Failure
The question of how long a person can live with left heart failure is complex and depends on various factors. While some individuals may live for many years with appropriate management, others may experience a more rapid decline in health. It’s essential to note that predicting life expectancy in individual cases is challenging, and healthcare providers typically provide a range rather than a specific number of years.
Statistical Data and Survival Rates
Survival rates for left heart failure have improved over the years due to advancements in medical treatment and management strategies. According to data from the American Heart Association (AHA), the five-year survival rate for heart failure patients is approximately 50%. However, these statistics are generalized and may not reflect individual experiences.
Stage-Based Prognosis
Left heart failure is often classified into stages based on the severity of symptoms and functional limitations. The stages, as defined by the American College of Cardiology (ACC) and the American Heart Association (AHA), include:
1. Stage A: Patients at high risk for heart failure but without structural heart disease or symptoms.
2. Stage B: Patients with structural heart disease (such as left ventricular hypertrophy) but without symptoms of heart failure.
3. Stage C: Patients with structural heart disease and current or prior symptoms of heart failure.
4. Stage D: Patients with advanced heart failure requiring specialized interventions, such as mechanical circulatory support or heart transplantation.
The prognosis varies significantly between these stages, with earlier stages generally associated with better outcomes and longer life expectancy.
Individualized Prognosis
While statistical data and stage-based classifications provide a general overview, predicting an individual’s life expectancy requires a personalized approach. Healthcare providers consider the patient’s unique medical history, current symptoms, response to treatment, and overall health status when discussing prognosis.
Improving Prognosis and Quality of Life
While left heart failure can have a significant impact on life expectancy, there are strategies to improve prognosis and enhance quality of life for patients:
1. Medication Management: Proper use of medications, including ACE inhibitors, beta-blockers, diuretics, and aldosterone antagonists, can help improve heart function, reduce symptoms, and prolong life.
2. Lifestyle Modifications: Adopting a heart-healthy lifestyle, including regular exercise, a balanced diet low in sodium and saturated fats, smoking cessation, and weight management, can positively impact prognosis.
3. Regular Monitoring: Regular follow-up appointments with healthcare providers allow for ongoing monitoring of heart function, symptom management, and adjustments to treatment plans as needed.
4. Advanced Therapies: In advanced cases of heart failure, advanced therapies such as CRT, ICDs, ventricular assist devices (VADs), or heart transplantation may be considered to improve prognosis and quality of life.
5. Patient Education and Support: Educating patients and their families about heart failure, treatment options, self-care strategies, and symptom recognition empowers individuals to actively participate in their care and make informed decisions.
6. Psychosocial Support: Addressing psychosocial factors such as stress, anxiety, and depression through counseling, support groups, or therapy can improve overall well-being and quality of life.
Conclusion
Left heart failure is a chronic condition that requires ongoing management and support. While life expectancy can vary widely among individuals with left heart failure, advances in medical treatment and comprehensive care strategies have improved outcomes and quality of life for many patients. By understanding the factors that influence prognosis, implementing evidence-based interventions, and fostering a collaborative approach between patients, healthcare providers, and caregivers, it’s possible to navigate left heart failure effectively and optimize outcomes for those affected by this condition.