Ventricular tachycardia (VT) is a serious cardiac rhythm disorder characterized by rapid, abnormal electrical activity in the heart’s lower chambers (ventricles). This condition can pose significant risks to an individual’s health and well-being, potentially leading to life-threatening complications if not properly managed. In this article, we will delve into the reasons why ventricular tachycardia is dangerous, exploring its mechanisms, associated risks, and the importance of timely medical intervention.
Before delving into its dangers, let’s first understand what ventricular tachycardia entails. In a normal heartbeat, electrical impulses originate in the heart’s natural pacemaker (the sinoatrial node) and travel through specific pathways to coordinate the heart’s contractions. However, in ventricular tachycardia, abnormal electrical signals disrupt this process, causing the ventricles to contract too quickly and inefficiently.
Mechanisms of Ventricular Tachycardia
The mechanisms underlying ventricular tachycardia can vary, but they often involve abnormalities in the heart’s electrical system. These abnormalities can result from structural heart disease, such as coronary artery disease, cardiomyopathy, or previous heart attacks. Additionally, imbalances in electrolytes or disruptions in the heart’s normal conduction pathways can contribute to the development of ventricular tachycardia.
The Dangers Unleashed
1. Hemodynamic Instability: One of the primary dangers of ventricular tachycardia is its potential to cause hemodynamic instability. The rapid and erratic ventricular contractions can lead to a significant decrease in cardiac output, impairing the heart’s ability to pump an adequate amount of blood to vital organs. This can result in symptoms such as dizziness, lightheadedness, and in severe cases, loss of consciousness.
2. Risk of Ventricular Fibrillation: Ventricular tachycardia can degenerate into a more chaotic and life-threatening rhythm known as ventricular fibrillation (VF). In VF, the ventricles quiver rather than contract effectively, leading to a complete cessation of effective blood flow. Without immediate intervention such as defibrillation, VF can rapidly progress to sudden cardiac arrest and death.
3. Increased Risk of Stroke: Prolonged episodes of ventricular tachycardia can also increase the risk of stroke. The irregular heart rhythm can promote the formation of blood clots within the heart chambers, particularly in individuals with pre-existing conditions such as atrial fibrillation or structural heart disease. These blood clots can then dislodge and travel to the brain, causing a stroke.
4. Worsening Heart Failure: Ventricular tachycardia can exacerbate heart failure, a condition where the heart struggles to pump blood effectively. The increased workload placed on the heart during tachycardic episodes can lead to further deterioration of cardiac function, worsening symptoms such as shortness of breath, fatigue, and fluid retention.
5. Electrical Storms: In some cases, ventricular tachycardia can trigger recurrent and frequent episodes of rapid heart rhythms, known as electrical storms. These storms can be challenging to manage and may require aggressive medical interventions, including antiarrhythmic medications, implantable cardioverter-defibrillators (ICDs), or catheter ablation procedures.
Diagnostic and Treatment Approaches
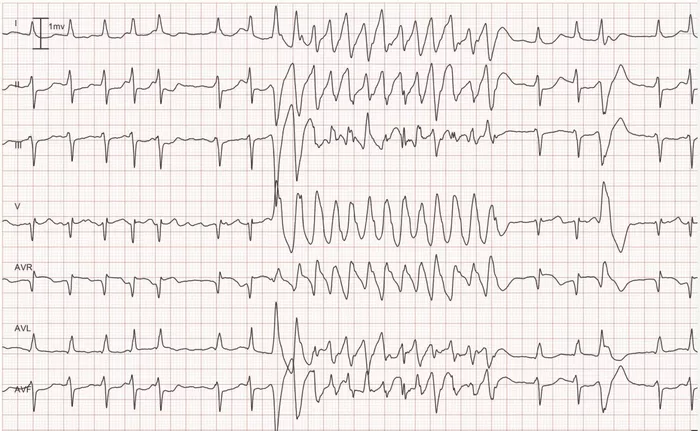
Diagnosing ventricular tachycardia typically involves a combination of clinical assessment, electrocardiography (ECG), and cardiac imaging studies. Once diagnosed, the management of ventricular tachycardia aims to restore normal heart rhythm, prevent recurrence, and reduce the risk of complications.
1. Antiarrhythmic Medications: Medications such as amiodarone, lidocaine, and beta-blockers may be prescribed to help control ventricular tachycardia and reduce the likelihood of recurrence.
2. Implantable Cardioverter-Defibrillators (ICDs): For individuals at high risk of life-threatening arrhythmias, implanting an ICD can provide rapid detection and termination of ventricular tachycardia or fibrillation through electrical shocks.
3. Catheter Ablation: In cases where medications and ICDs are insufficient, catheter ablation procedures may be recommended. During ablation, a catheter is used to target and eliminate abnormal heart tissue responsible for generating the arrhythmia.
4. Lifestyle Modifications: Adopting a heart-healthy lifestyle, including regular exercise, a balanced diet, smoking cessation, and managing underlying medical conditions such as hypertension and diabetes, can also play a crucial role in managing ventricular tachycardia.
Conclusion
In conclusion, ventricular tachycardia poses significant dangers to cardiovascular health, ranging from hemodynamic instability and increased risk of ventricular fibrillation to potential stroke and worsening heart failure. Prompt diagnosis, appropriate management strategies, and lifestyle modifications are key to mitigating these risks and improving outcomes for individuals with this condition. Early recognition of symptoms, regular cardiac monitoring, and collaboration between patients, healthcare providers, and cardiac specialists are essential components of effective ventricular tachycardia management.