The heart is a complex organ responsible for pumping blood throughout the body, ensuring oxygen and nutrients reach every cell. One crucial parameter in assessing heart function is the ejection fraction (EF) of the left ventricle (LV). This article aims to delve into the concept of EF, explore what constitutes a normal EF of the LV, its clinical significance, measurement methods, and factors influencing EF.
Ejection Fraction Explained
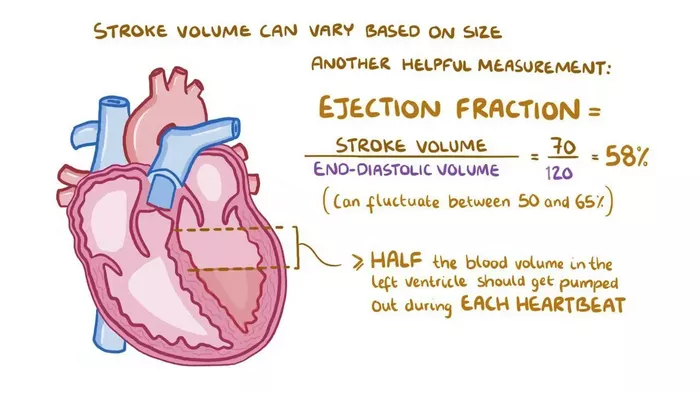
Ejection fraction refers to the percentage of blood pumped out of the left ventricle with each heartbeat. It is a vital indicator of cardiac performance, reflecting the heart’s ability to efficiently eject blood into circulation. EF is typically expressed as a percentage and can be calculated using various imaging techniques such as echocardiography, cardiac magnetic resonance imaging (MRI), or nuclear medicine scans.
Normal Ejection Fraction Range
The normal range for LV ejection fraction is generally considered to be between 50% and 70%. This means that during each contraction of the heart, approximately half to two-thirds of the blood in the left ventricle is pumped out into the systemic circulation. An EF below 50% may indicate reduced heart function and is often associated with conditions such as heart failure, myocardial infarction, or cardiomyopathy.
Clinical Significance of Ejection Fraction
Understanding the ejection fraction of the left ventricle is crucial in several clinical contexts. Firstly, it helps diagnose and classify heart failure, with EF being a key criterion in differentiating between heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF). HFrEF is characterized by an EF below 40-50%, indicating impaired systolic function, while HFpEF involves diastolic dysfunction with a preserved EF.
Moreover, EF assessment is essential in monitoring patients with cardiovascular diseases, assessing response to treatment, and predicting outcomes. A lower EF is associated with a higher risk of adverse events such as arrhythmias, heart failure exacerbations, and mortality. On the other hand, a normal or improved EF following interventions like medications, revascularization procedures, or cardiac rehabilitation is indicative of better prognosis.
Methods of Ejection Fraction Measurement
Several imaging modalities can be employed to measure ejection fraction accurately. Echocardiography, a non-invasive and widely available technique, uses ultrasound waves to visualize the heart’s structures and assess its function, including EF. Cardiac MRI provides detailed images of cardiac anatomy and function, offering high accuracy in EF measurement, especially in challenging cases or when echocardiography results are inconclusive.
Nuclear medicine techniques such as radionuclide ventriculography or gated single-photon emission computed tomography (SPECT) are also utilized for EF evaluation. These methods involve injecting a radioactive tracer into the bloodstream, which is then detected by a gamma camera to create images showing cardiac function and EF.
Factors Influencing Ejection Fraction
Several factors can influence ejection fraction measurements, leading to variations in EF values or affecting the interpretation of results. For instance, age-related changes in myocardial contractility and compliance can impact EF, with older individuals often exhibiting lower EF values even in the absence of cardiac pathology. Similarly, comorbidities like hypertension, diabetes, and chronic kidney disease can contribute to alterations in EF.
Furthermore, medications such as beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin receptor blockers (ARBs) can modulate EF by improving cardiac function, reducing afterload, and preventing remodeling processes. Conversely, certain drugs like chemotherapy agents may have cardiotoxic effects, leading to decreased EF and cardiac dysfunction.
Clinical Implications and Management
In clinical practice, the interpretation of ejection fraction results must be contextualized within the patient’s overall clinical picture, including symptoms, medical history, and other diagnostic findings. Patients with reduced EF indicative of heart failure require comprehensive management strategies aimed at improving symptoms, preventing disease progression, and reducing cardiovascular events.
Treatment approaches for heart failure with reduced EF often include guideline-directed medical therapies such as beta-blockers, ACE inhibitors or ARBs, angiotensin receptor-neprilysin inhibitors (ARNIs), diuretics, and mineralocorticoid receptor antagonists (MRAs). In addition to pharmacological interventions, lifestyle modifications, dietary adjustments, regular exercise, and close monitoring are integral components of heart failure management.
For patients with borderline EF or those at risk of developing heart failure, early identification of predisposing factors, aggressive risk factor modification, and regular follow-up are essential to prevent disease onset or progression. Moreover, interventions targeting reversible causes of reduced EF, such as coronary artery disease requiring revascularization or valvular heart disease necessitating surgical correction, can lead to EF improvement and better outcomes.
Conclusion
Ejection fraction of the left ventricle plays a pivotal role in assessing cardiac function, diagnosing heart failure, guiding treatment decisions, and predicting outcomes in cardiovascular diseases. Understanding the normal range of EF, measurement techniques, factors influencing EF values, and clinical implications is imperative for healthcare professionals involved in managing patients with cardiac conditions. By integrating EF assessment into comprehensive cardiovascular evaluations and adopting evidence-based therapeutic strategies, clinicians can optimize patient care, enhance quality of life, and improve cardiovascular outcomes.