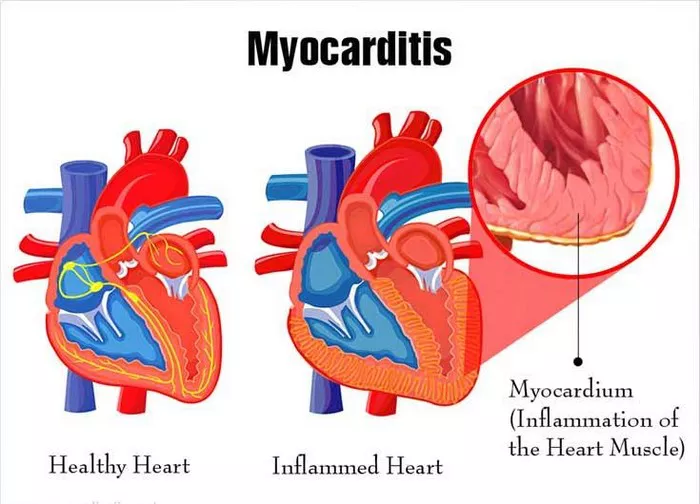
Autoimmune myocarditis is a condition characterized by inflammation of the heart muscle caused by an autoimmune response, where the body’s immune system mistakenly attacks the heart tissue. Diagnosing autoimmune myocarditis involves a comprehensive approach that combines clinical evaluation, laboratory tests, imaging studies, and sometimes invasive procedures. This article explores the various methods and techniques used in the diagnosis of autoimmune myocarditis.
Clinical Evaluation
The initial step in diagnosing autoimmune myocarditis involves a thorough clinical evaluation by a healthcare provider. This evaluation typically includes:
1. Medical History: The healthcare provider will take a detailed medical history, including symptoms, past medical conditions, medications, family history of heart disease, and any recent infections or exposures that may be relevant to the development of myocarditis.
2. Physical Examination: A physical examination may reveal signs such as an abnormal heart rhythm (arrhythmia), heart murmurs, fluid retention (edema), or signs of heart failure.
3. Symptom Assessment: Symptoms of autoimmune myocarditis can vary but may include chest pain, shortness of breath, fatigue, palpitations, and in severe cases, signs of heart failure such as fluid buildup in the lungs (pulmonary edema) or swelling in the legs (peripheral edema).
Laboratory Tests
Several laboratory tests are commonly used in the diagnosis of autoimmune myocarditis:
1. Blood Tests: Blood tests can help assess markers of inflammation, cardiac enzymes (such as troponin and creatine kinase-MB), autoimmune markers (such as antinuclear antibodies and anti-myosin antibodies), and markers of heart function (such as brain natriuretic peptide or BNP).
2. Electrolyte Levels: Abnormalities in electrolyte levels, such as potassium and magnesium, may be observed in myocarditis and can contribute to arrhythmias.
3. Inflammatory Markers: Elevated levels of inflammatory markers, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), may indicate ongoing inflammation in the heart.
4. Viral Testing: Since viral infections can sometimes trigger myocarditis, testing for specific viruses (such as enteroviruses, adenoviruses, or parvovirus B19) may be conducted through PCR (polymerase chain reaction) or serological tests.
Imaging Studies
Imaging studies play a crucial role in the diagnosis and assessment of autoimmune myocarditis. Common imaging modalities include:
1. Echocardiography: Echocardiography uses sound waves to create images of the heart and can help evaluate heart function, detect abnormalities such as ventricular dysfunction or enlargement, assess for pericardial effusion (fluid around the heart), and look for signs of inflammation or myocardial damage.
2. Cardiac MRI: Cardiac magnetic resonance imaging (MRI) provides detailed images of the heart’s structure, function, and tissue characteristics. It is particularly useful in detecting myocardial inflammation (edema) and fibrosis, as well as assessing for myocardial damage and overall cardiac function.
3. CT Scan: Computed tomography (CT) scans may be used to evaluate the heart’s anatomy, assess for coronary artery disease, and rule out other cardiac conditions that may mimic myocarditis.
Invasive Procedures
In some cases, invasive procedures may be necessary to confirm the diagnosis of autoimmune myocarditis or obtain additional information:
1. Endomyocardial Biopsy: Endomyocardial biopsy involves obtaining a small tissue sample from the heart muscle, usually from the right ventricle, using a catheter-based approach. The tissue sample is then examined under a microscope to look for inflammatory infiltrates, fibrosis, and other abnormalities indicative of myocarditis. However, endomyocardial biopsy is not always performed due to its invasive nature and potential risks.
2. Electrophysiological Studies: Electrophysiological studies, such as cardiac electrophysiology testing or electrophysiological mapping, may be conducted to assess for arrhythmias or conduction abnormalities associated with myocarditis.
Differential Diagnosis
It’s important to note that autoimmune myocarditis can mimic other cardiac conditions, and a differential diagnosis may be necessary to distinguish it from:
- Viral myocarditis
- Dilated cardiomyopathy
- Hypertrophic cardiomyopathy
- Acute coronary syndrome
- Pericarditis
- Myocardial infarction
Conclusion
Diagnosing autoimmune myocarditis requires a multi-faceted approach that integrates clinical evaluation, laboratory tests, imaging studies, and occasionally invasive procedures. Collaboration between healthcare providers, including cardiologists, immunologists, and pathologists, is essential for accurate diagnosis and appropriate management of this challenging condition. Early diagnosis and treatment are crucial to improving outcomes and preventing long-term complications associated with autoimmune myocarditis.