Premature Ventricular Contractions (PVCs) are a common cardiac arrhythmia that affects many individuals worldwide. These abnormal heartbeats can cause significant concern and anxiety, leading individuals to wonder if PVCs will ever go away or if they require medical intervention. In this comprehensive article, we delve into the nature of PVCs, their potential causes, risk factors, diagnostic procedures, treatment options, and prognosis to provide a thorough understanding of this condition.
Premature Ventricular Contractions occur when the heart’s ventricles contract prematurely, leading to an irregular heartbeat. Instead of following the normal electrical pathway through the heart’s chambers, an extra electrical impulse originates in the ventricles, causing them to contract too soon. This disruption can be felt as a palpitation, skipped beat, or fluttering sensation in the chest.
It’s important to note that occasional PVCs are common and often benign, especially in healthy individuals without underlying heart conditions. However, frequent or persistent PVCs may indicate an underlying issue that requires medical attention.
Causes of PVCs
Several factors can contribute to the development of PVCs, including:
1. Stress and Anxiety: Emotional stress and anxiety can trigger PVCs in susceptible individuals.
2. Caffeine and Stimulants: Excessive consumption of caffeine, nicotine, or other stimulants can increase the likelihood of PVCs.
3. Electrolyte Imbalances: Low levels of potassium, magnesium, or calcium in the blood can disrupt normal heart rhythm and contribute to PVCs.
4. Heart Conditions: Certain heart conditions such as coronary artery disease, heart failure, or cardiomyopathy can predispose individuals to PVCs.
5. Medications: Some medications, including certain asthma medications, decongestants, and antiarrhythmic drugs, may trigger PVCs as a side effect.
Identifying and addressing the underlying cause of PVCs is crucial in managing the condition effectively.
Risk Factors for PVCs
While PVCs can occur in individuals of any age, certain risk factors may increase the likelihood of experiencing PVCs:
1. Age: The risk of PVCs tends to increase with age, particularly beyond the age of 50.
2. Heart Disease: Individuals with existing heart conditions, such as coronary artery disease or heart failure, are at higher risk of developing PVCs.
3. High Blood Pressure: Hypertension can contribute to cardiac arrhythmias, including PVCs.
4. Stimulant Use: Excessive consumption of caffeine, tobacco, or other stimulants can trigger PVCs.
5. Stress and Anxiety: Emotional stress and anxiety can exacerbate PVCs in susceptible individuals.
Understanding these risk factors can help individuals take proactive steps to reduce their risk and manage PVCs effectively.
Diagnostic Procedures
When evaluating PVCs, healthcare providers may recommend the following diagnostic procedures:
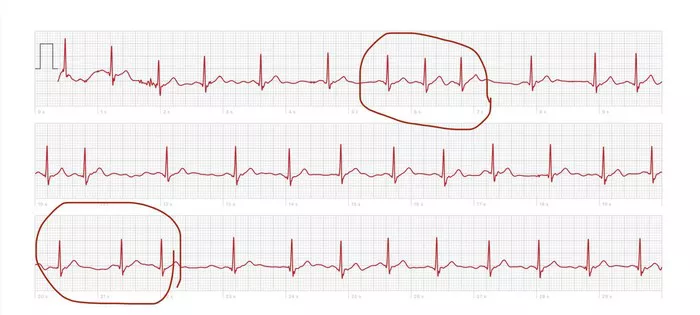
1. Electrocardiogram (ECG or EKG): An ECG records the heart’s electrical activity and can detect abnormalities such as PVCs.
2. Holter Monitor: A portable device worn for 24 to 48 hours to monitor heart activity continuously, providing a more comprehensive assessment of PVC frequency and patterns.
3. Event Monitor: Similar to a Holter monitor but worn for a longer duration, typically up to 30 days, to capture intermittent PVCs.
4. Echocardiogram: This imaging test uses sound waves to create a detailed picture of the heart’s structure and function, helping to evaluate for underlying heart conditions.
5. Stress Test: Involves exercising on a treadmill or stationary bike while being monitored for changes in heart rhythm, which can unmask PVCs that occur during physical activity.
These diagnostic tests help healthcare providers determine the severity of PVCs, assess underlying heart function, and guide treatment decisions.
Treatment Options for PVCs
The approach to treating PVCs depends on several factors, including the frequency and severity of the arrhythmia, underlying health conditions, and the presence of symptoms. Treatment options may include:
1. Lifestyle Modifications: Making lifestyle changes can help reduce PVC frequency and severity. These changes may include reducing caffeine and stimulant intake, managing stress through relaxation techniques or counseling, maintaining a healthy diet, exercising regularly, and avoiding tobacco and excessive alcohol consumption.
2. Medications: In some cases, medications such as beta-blockers, calcium channel blockers, or antiarrhythmic drugs may be prescribed to suppress PVCs and restore normal heart rhythm. However, medication therapy is typically reserved for individuals with frequent or symptomatic PVCs.
3. Catheter Ablation: Ablation therapy involves the insertion of thin, flexible tubes (catheters) into the heart to deliver radiofrequency energy or cryotherapy to areas responsible for generating abnormal electrical impulses. This procedure aims to eliminate the source of PVCs and restore normal heart rhythm. 4. Implantable Cardioverter-Defibrillator (ICD): In rare cases where PVCs are associated with a high risk of life-threatening arrhythmias, an ICD may be implanted to monitor heart rhythm continuously and deliver electrical shocks if needed to restore normal rhythm.
Cardiac Rehabilitation: For individuals with underlying heart conditions contributing to PVCs, cardiac rehabilitation programs can provide structured exercise, education, and support to improve heart health and reduce arrhythmia risk.
The choice of treatment will be individualized based on the patient’s specific circumstances and medical history.
Prognosis and Outlook
The prognosis for individuals with PVCs is generally favorable, especially when PVCs are infrequent, asymptomatic, and not associated with underlying heart disease. Making lifestyle modifications, managing stress, and following a healthy lifestyle can significantly reduce PVC frequency and improve overall heart health.
However, for individuals with frequent or symptomatic PVCs, close monitoring by healthcare providers is essential to assess response to treatment, identify any complications, and adjust the management plan as needed. With appropriate medical care and lifestyle management, many individuals with PVCs can lead active and fulfilling lives.
Conclusion
Premature Ventricular Contractions (PVCs) are a common cardiac arrhythmia that can cause significant concern for affected individuals. While occasional PVCs are often benign, frequent or symptomatic PVCs may require medical evaluation and treatment. Understanding the causes, risk factors, diagnostic procedures, treatment options, and prognosis for PVCs is essential in managing this condition effectively.
By working closely with healthcare providers, making lifestyle modifications, and following a personalized treatment plan, individuals with PVCs can reduce arrhythmia frequency, improve heart health, and achieve a positive outlook for their cardiovascular well-being. Early detection, intervention, and proactive management play key roles in optimizing outcomes for individuals with PVCs, highlighting the importance of comprehensive cardiac care in promoting heart health and quality of life.