Cholesterol and hyperlipidemia are terms often used interchangeably in discussions about heart health and lipid levels. However, they are not synonymous and understanding the difference between them is crucial for effective management and treatment. In this comprehensive article, we will delve into the definitions, causes, symptoms, risk factors, diagnosis, and management strategies for high cholesterol and hyperlipidemia.
What is High Cholesterol?
Cholesterol is a waxy, fat-like substance found in the cells of the body and certain foods. It plays a vital role in building healthy cells, producing hormones, and aiding in digestion. Cholesterol travels through the bloodstream in lipoproteins, which are a combination of fats (lipids) and proteins. The two main types of lipoproteins that carry cholesterol are low-density lipoprotein (LDL) and high-density lipoprotein (HDL).
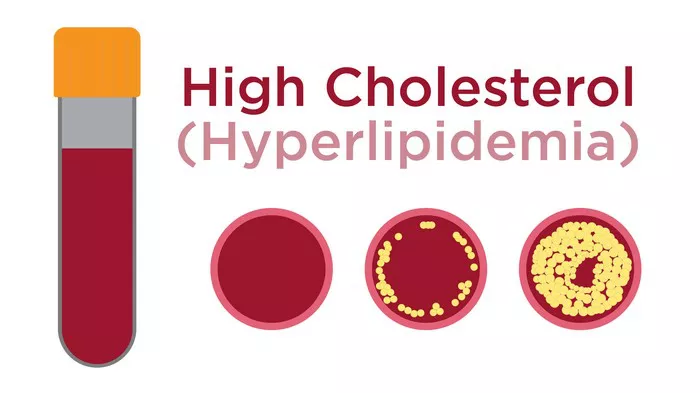
High cholesterol, also known as hypercholesterolemia, refers to elevated levels of cholesterol in the blood, specifically high levels of LDL cholesterol. Having high LDL cholesterol can lead to the buildup of plaque in the arteries, a condition known as atherosclerosis, which increases the risk of heart disease and stroke.
What is Hyperlipidemia?
Hyperlipidemia is a broader term that encompasses elevated levels of lipids (fats) in the blood, including cholesterol and triglycerides. It includes conditions characterized by high levels of LDL cholesterol, low levels of HDL cholesterol, or elevated triglycerides, or a combination of these lipid abnormalities. Hyperlipidemia can be further classified based on the specific lipid(s) that are elevated.
Causes of High Cholesterol and Hyperlipidemia
High Cholesterol Causes:
1. Diet: Consuming foods high in saturated and trans fats can increase LDL cholesterol levels.
2. Genetics: Familial hypercholesterolemia is an inherited condition that leads to high cholesterol levels from birth.
3. Lack of exercise: Physical inactivity can contribute to high LDL cholesterol and low HDL cholesterol levels.
4. Obesity: Being overweight or obese can disrupt lipid metabolism and lead to elevated cholesterol levels.
5. Age and gender: Cholesterol levels tend to rise with age, and women may experience changes in cholesterol levels during menopause.
Hyperlipidemia Causes:
1. Genetics: Inherited disorders such as familial combined hyperlipidemia can cause abnormalities in lipid metabolism.
2. Diabetes: Uncontrolled diabetes can lead to high triglyceride levels and low HDL cholesterol levels.
3. Hypothyroidism: An underactive thyroid gland can affect lipid levels, leading to hyperlipidemia.
4. Kidney disease: Impaired kidney function can alter lipid metabolism and contribute to hyperlipidemia.
5. Medications: Certain medications such as corticosteroids, diuretics, and some antipsychotics can affect lipid levels.
Symptoms of High Cholesterol and Hyperlipidemia
High cholesterol and hyperlipidemia are often asymptomatic, meaning they do not cause noticeable symptoms in the early stages. However, as these conditions progress and lead to complications such as atherosclerosis, symptoms may manifest. Some possible symptoms include:
- Chest pain or discomfort (angina) due to reduced blood flow to the heart.
- Leg pain or cramping (claudication) caused by peripheral artery disease.
- Shortness of breath, fatigue, or weakness, especially during physical exertion.
- Yellowish deposits of cholesterol around the eyes (xanthomas) or under the skin (xanthelasma).
It’s important to note that symptoms may vary depending on the severity of the condition and the presence of underlying cardiovascular diseases.
Risk Factors for High Cholesterol and Hyperlipidemia
High Cholesterol Risk Factors:
1. Unhealthy diet: Consuming foods high in saturated fats, trans fats, and cholesterol.
2. Lack of physical activity: Sedentary lifestyle contributes to weight gain and lipid abnormalities.
3. Smoking: Tobacco use damages blood vessels and promotes atherosclerosis.
4. Family history: Genetics can influence cholesterol levels and increase the risk of familial hypercholesterolemia.
5. Age and gender: Men typically have higher cholesterol levels than premenopausal women, but women’s risk increases after menopause.
Hyperlipidemia Risk Factors:
1. Genetic predisposition: Inherited lipid disorders such as familial hyperlipidemia.
2. Obesity: Excess body weight and abdominal fat can lead to dyslipidemia.
3. Diabetes: Poorly controlled diabetes can cause dyslipidemia, especially high triglycerides and low HDL cholesterol.
4. Sedentary lifestyle: Lack of exercise and physical activity contributes to abnormal lipid profiles.
5. Certain medical conditions: Hypothyroidism, kidney disease, and liver disease can affect lipid metabolism.
Diagnosis of High Cholesterol and Hyperlipidemia
High Cholesterol Diagnosis:
1. Blood tests: A lipid profile measures total cholesterol, LDL cholesterol, HDL cholesterol, and triglyceride levels.
2. Risk assessment: Factors such as age, gender, family history, smoking, and medical conditions are considered in assessing cardiovascular risk.
3. Imaging tests: Coronary angiography or CT scans may be done to evaluate the extent of atherosclerosis.
Hyperlipidemia Diagnosis:
1. Lipid panel: Similar to high cholesterol diagnosis, a lipid panel measures cholesterol (total, LDL, HDL) and triglyceride levels.
2. Genetic testing: In cases of suspected inherited lipid disorders, genetic testing may be recommended.
3. Additional tests: Thyroid function tests, kidney function tests, and liver function tests may be performed to identify underlying causes of hyperlipidemia.
Management Strategies for High Cholesterol and Hyperlipidemia
Lifestyle Modifications:
1. Healthy diet: Focus on fruits, vegetables, whole grains, lean proteins, and foods low in saturated and trans fats.
2. Regular exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
3. Weight management: Maintain a healthy weight through balanced diet and physical activity.
4. Smoking cessation: Quitting smoking reduces cardiovascular risk and improves lipid profiles.
Medications:
1. Statins: These are commonly prescribed to lower LDL cholesterol and reduce the risk of cardiovascular events.
2. Other cholesterol-lowering drugs: Ezetimibe, PCSK9 inhibitors, bile acid sequestrants, and fibrates may be used in combination with statins or as alternatives.
3. Triglyceride-lowering medications: Omega-3 fatty acids, fibrates, and niacin can help lower triglyceride levels.
Diabetes management: Tight control of blood sugar levels is essential for diabetic patients with hyperlipidemia.
Monitoring and Follow-Up:
1. Regular check-ups: Monitor lipid levels, blood pressure, and other cardiovascular risk factors regularly.
2. Adjustments to treatment: Based on response to treatment and changes in risk factors, medication doses may be adjusted.
3. Lifestyle counseling: Educate patients on healthy habits, dietary choices, and adherence to medication regimens.
Conclusion
Hyperlipidemia is a broader term that refers to elevated levels of lipids (fats) in the blood, including cholesterol and triglycerides. On the other hand, high cholesterol specifically focuses on elevated levels of LDL cholesterol, which is a type of lipid. In essence, hyperlipidemia encompasses a wider range of lipid abnormalities, while high cholesterol targets a specific type of cholesterol that contributes to cardiovascular risk.