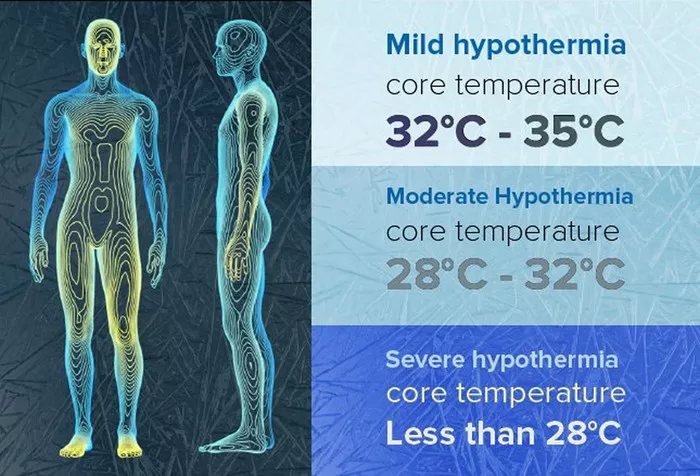
In the intricate dance of human physiology, the heart plays the leading role, orchestrating the ebb and flow of life with every beat. Yet, like any finely tuned instrument, its performance can falter under extreme conditions. Hypothermia, a condition where the body’s core temperature falls below 35°C (95°F), presents such an extremity, challenging the heart’s rhythm and potentially leading to arrhythmias. This article delves into the physiological cascades triggered by hypothermia, exploring how and why these can culminate in arrhythmic events, and underscores the importance of understanding and mitigating these effects in clinical practice and emergency response.
The Cold Stress Response
Hypothermia sets off a chain reaction within the body, aimed initially at preserving core temperature to protect vital organs. This cold stress response includes mechanisms such as peripheral vasoconstriction, shivering, and alterations in metabolic rate. However, as core temperature continues to drop, these responses can have unintended consequences on cardiac function.
Peripheral Vasoconstriction and Its Cardiac Impacts
One of the body’s first defenses against cold is peripheral vasoconstriction, the narrowing of blood vessels in the skin and extremities. This response reduces heat loss but increases vascular resistance, placing additional strain on the heart. The heart must work harder to pump blood through these narrowed vessels, a challenge that can exacerbate underlying cardiac conditions and lead to increased blood pressure and potential myocardial ischemia in susceptible individuals.
Metabolic Shifts and Electrolyte Imbalance
As the body’s temperature continues to fall, metabolic changes ensue, aimed at generating heat. These include increased glycolysis and fat metabolism. However, these processes can lead to an accumulation of metabolic byproducts, such as lactate, and alter the body’s acid-base balance, leading to metabolic acidosis. Hypothermia also disrupts the normal balance of electrolytes, crucial for heart and muscle function. Potassium, calcium, and magnesium levels can fluctuate, directly impacting the heart’s electrical activity and increasing the risk of arrhythmias.
The Hypothermic Heart: Electrical Instability and Arrhythmias
At the core of the relationship between hypothermia and arrhythmias is the heart’s electrical instability as body temperature drops. Hypothermia affects the heart’s electrical conduction system, slowing the rate of depolarization and repolarization. This slowing can lead to prolonged intervals on the electrocardiogram (ECG), such as the PR, QRS, and QT intervals, creating a ripe environment for arrhythmic events.
Bradyarrhythmias
As the heart slows in response to cooling, bradyarrhythmias (abnormally slow heart rates) are common. Sinus bradycardia is often seen in mild to moderate hypothermia, while more severe cooling can lead to atrioventricular blocks. These conditions result from the delayed conduction of electrical impulses through the heart, compromising its ability to pump efficiently and deliver adequate oxygen to the body.
Atrial and Ventricular Arrhythmias
Atrial fibrillation, a disorder characterized by rapid and irregular beating of the atrial chambers, can occur, particularly as the body transitions from a hypothermic to a rewarmed state. This state increases the risk of stroke and other complications if not managed carefully. Ventricular arrhythmias, including ventricular tachycardia and ventricular fibrillation, represent the most dangerous sequelae of hypothermia. These arrhythmias can lead to sudden cardiac death if not promptly addressed.
The Unique Phenomenon of J Waves
A hallmark of hypothermia on an ECG is the presence of J waves (also known as Osborn waves). These deflections at the junction of the QRS complex and the ST segment are thought to result from the differential effects of cooling on the epicardial and endocardial surfaces of the heart. While not harmful in themselves, J waves serve as a biomarker for hypothermia and a predictor of the potential for more serious arrhythmias.
Rewarming: A Double-Edged Sword
The process of rewarming a hypothermic patient must be carefully managed to avoid triggering or exacerbating arrhythmias. Rapid changes in temperature can cause vasodilation, leading to hypotension and a sudden influx of cold, acidotic blood to the heart, further destabilizing its electrical activity. Controlled, gradual rewarming is essential to minimize these risks, allowing the body to adjust and restore normal metabolic and electrical functions.
Preventive Measures and Treatment Strategies
Prevention of hypothermia is paramount, particularly in environments where exposure to cold is a risk. Adequate clothing, shelter, and the avoidance of alcohol, which can accelerate heat loss, are simple yet effective strategies. In the clinical setting, early recognition and treatment of hypothermia can prevent the onset of arrhythmias. This includes continuous monitoring of core temperature and cardiac rhythms, gradual rewarming techniques, and the correction of electrolyte imbalances and acidosis. Pharmacological interventions may be necessary to manage arrhythmias if they occur, but the underlying hypothermia must be addressed to resolve the root cause of the problem.
Conclusion
The link between hypothermia and arrhythmia is a complex interplay of physiological responses to cold stress. While these responses are initially adaptive, aimed at preserving core body temperature, their impact on the heart can lead to dangerous and potentially fatal arrhythmias. Understanding the mechanisms behind these effects is crucial for healthcare providers, emergency responders, and individuals in cold environments to prevent, recognize, and treat these conditions effectively. As research continues to unravel the mysteries of the hypothermic heart, the prospects for improved management and outcomes in affected patients look increasingly promising.