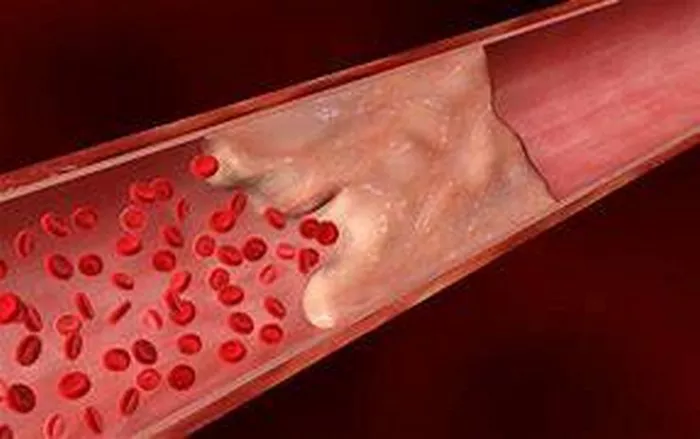
Calcification in heart arteries, also known as coronary artery calcification (CAC), is a common finding in cardiovascular disease. It refers to the buildup of calcium deposits in the walls of the coronary arteries, which supply oxygen-rich blood to the heart muscle. This condition can lead to atherosclerosis, a narrowing and hardening of the arteries that can increase the risk of heart attacks and other cardiovascular events. In this article, we will explore the causes of calcification in heart arteries, the risk factors associated with this condition, and the implications for cardiovascular health.
What is Coronary Artery Calcification?
Coronary artery calcification occurs when calcium deposits accumulate in the walls of the coronary arteries. These deposits can be detected and quantified using imaging techniques such as computed tomography (CT) scans. A coronary artery calcium (CAC) score is often used to assess the extent of calcification and estimate the risk of coronary artery disease (CAD) and cardiovascular events.
Causes of Coronary Artery Calcification:
1. Atherosclerosis: The primary cause of coronary artery calcification is atherosclerosis, a condition characterized by the buildup of plaque in the arteries. Plaque is composed of cholesterol, fatty substances, cellular waste, calcium, and other substances. Over time, the plaque can harden and calcify, leading to narrowing of the arteries and reduced blood flow to the heart.
2. High Cholesterol Levels: Elevated levels of LDL cholesterol (“bad” cholesterol) in the blood can contribute to the formation of plaque in the arteries. When LDL cholesterol oxidizes, it becomes more likely to be deposited in the arterial walls, contributing to the development of atherosclerosis and calcification.
3. Hypertension (High Blood Pressure): Chronic high blood pressure can damage the inner lining of the arteries, making them more susceptible to plaque buildup and calcification. The increased pressure within the arteries can also lead to mechanical stress and injury, further promoting the development of atherosclerosis.
4. Smoking: Tobacco smoke contains harmful chemicals that can damage blood vessels and promote inflammation. Smokers are at a higher risk of developing atherosclerosis and coronary artery calcification compared to non-smokers.
5. Diabetes: People with diabetes are more likely to develop atherosclerosis and coronary artery calcification. High blood sugar levels can damage the blood vessels and contribute to the formation of plaque in the arteries.
6. Obesity and Sedentary Lifestyle: Being overweight or obese, and leading a sedentary lifestyle, are risk factors for coronary artery calcification. Excess body fat, particularly around the abdomen, is associated with increased inflammation and insulin resistance, both of which can promote atherosclerosis.
7. Genetic Factors: Family history and genetics play a role in the development of coronary artery calcification. Some individuals may have a genetic predisposition to higher cholesterol levels, hypertension, or other risk factors for atherosclerosis.
8. Age and Gender: Advancing age is a significant risk factor for coronary artery calcification. As people age, the risk of developing atherosclerosis and calcification increases. Men are generally at a higher risk than premenopausal women, although the risk for women increases after menopause.
Implications for Cardiovascular Health:
Coronary artery calcification is a marker of underlying atherosclerosis and is associated with an increased risk of cardiovascular events such as heart attacks, strokes, and coronary artery disease. A high CAC score indicates a greater burden of calcification and suggests a higher risk of future cardiovascular events.
Prevention and Management:
1. Healthy Lifestyle: Adopting a healthy lifestyle can help prevent coronary artery calcification and reduce the risk of cardiovascular disease. This includes maintaining a balanced diet low in saturated fats and cholesterol, engaging in regular physical activity, maintaining a healthy weight, and avoiding tobacco use.
2. Control of Risk Factors: Managing risk factors such as high cholesterol, hypertension, diabetes, and obesity is essential in preventing coronary artery calcification. This may involve medications, lifestyle modifications, and regular monitoring of cardiovascular health.
3. Regular Screening: Regular screening for coronary artery calcification, using imaging techniques like CT scans, can help identify early signs of atherosclerosis and assess cardiovascular risk. Based on the findings, healthcare providers can develop personalized prevention and treatment strategies.
4. Medications: In some cases, medications such as statins (to lower cholesterol), blood pressure medications, and antiplatelet agents may be prescribed to reduce the progression of atherosclerosis and lower the risk of cardiovascular events.
Conclusion:
Coronary artery calcification is a common manifestation of atherosclerosis and is influenced by various risk factors including high cholesterol, hypertension, smoking, diabetes, obesity, genetics, age, and gender. Understanding the causes of calcification in heart arteries is crucial for preventing cardiovascular disease and promoting heart health. Lifestyle modifications, risk factor control, regular screening, and appropriate medical interventions play key roles in managing coronary artery calcification and reducing the risk of cardiovascular events.