Syncope, commonly known as fainting, is a transient loss of consciousness caused by a temporary reduction in blood flow to the brain. It can occur due to various reasons, including underlying medical conditions. One such condition often associated with syncope is heart failure. Heart failure is a chronic and progressive condition where the heart is unable to pump blood efficiently to meet the body’s needs. In this article, we will explore the relationship between syncope and heart failure, including its causes, symptoms, diagnosis, and management.
Understanding Heart Failure
Before delving into the connection between syncope and heart failure, it’s essential to have a basic understanding of heart failure itself. Heart failure occurs when the heart muscle becomes weakened or damaged, leading to a decrease in its pumping ability. As a result, the body may not receive an adequate supply of oxygen and nutrients carried by the blood.
Heart failure can be caused by various factors, including:
1. Coronary artery disease: A condition where the arteries supplying blood to the heart become narrowed or blocked, reducing blood flow to the heart muscle.
2. High blood pressure (hypertension): Prolonged high blood pressure can strain the heart muscle and lead to heart failure over time.
3. Cardiomyopathy: Diseases affecting the heart muscle can weaken the heart’s ability to pump effectively.
Heart valve disorders: Problems with heart valves can disrupt normal blood flow within the heart.
4. Myocarditis: Inflammation of the heart muscle can impair its function.
These are just a few examples of conditions that can contribute to the development of heart failure. It’s important to note that heart failure is a serious condition that requires medical management to improve symptoms and prevent complications.
Syncope: A Brief Overview
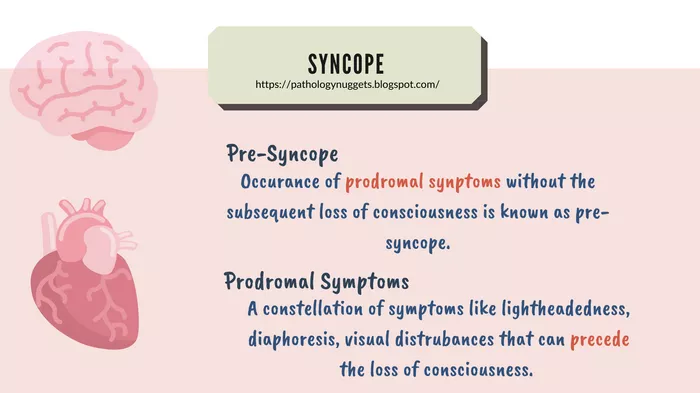
Syncope, as mentioned earlier, refers to a temporary loss of consciousness due to reduced blood flow to the brain. It is often described as “fainting” and can occur suddenly and without warning. Syncope can result from various causes, ranging from benign to potentially life-threatening. Some common causes of syncope include:
1. Vasovagal syncope: This is the most common type of syncope and is often triggered by emotional stress, pain, or standing for long periods. It occurs due to a sudden drop in heart rate and blood pressure.
2. Orthostatic hypotension: This type of syncope occurs when there is a significant drop in blood pressure upon standing up from a sitting or lying position.
3. Cardiac syncope: Syncope can also be caused by underlying heart conditions, such as arrhythmias (abnormal heart rhythms), structural heart defects, or heart valve disorders.
4. Neurological syncope: Certain neurological conditions can lead to syncope, such as seizures or transient ischemic attacks (TIAs).
It’s essential to determine the underlying cause of syncope as it can help guide appropriate treatment and management strategies.
Syncope as a Symptom of Heart Failure
In the context of heart failure, syncope can be a concerning symptom that warrants further evaluation. Syncope in individuals with heart failure can occur due to several reasons, including:
1. Reduced Cardiac Output: In heart failure, the heart’s ability to pump blood effectively is compromised. This reduced cardiac output can lead to decreased blood flow to the brain, resulting in syncope.
2. Arrhythmias: Heart failure can predispose individuals to develop abnormal heart rhythms or arrhythmias. Certain arrhythmias, such as ventricular tachycardia or bradycardia, can cause syncope.
3. Orthostatic Hypotension: Some medications used to manage heart failure can lower blood pressure, leading to orthostatic hypotension and potential syncope upon standing.
4. Underlying Structural Heart Disease: Heart failure often coexists with structural heart abnormalities, such as heart valve disorders or congenital heart defects. These abnormalities can contribute to syncope.
It’s important to note that syncope in individuals with heart failure may not always be directly related to the heart failure itself. Other factors, such as medication side effects, electrolyte imbalances, or concurrent medical conditions, can also contribute to syncope episodes.
Evaluating Syncope in Heart Failure Patients
When evaluating syncope in patients with known or suspected heart failure, healthcare providers typically conduct a comprehensive assessment to determine the underlying cause. This assessment may include:
1. Medical History: Gathering information about the patient’s medical history, including any previous episodes of syncope, heart failure diagnosis, medications, and other relevant conditions.
2. Physical Examination: A thorough physical examination can provide valuable insights, such as signs of fluid overload or heart murmurs indicative of structural heart abnormalities.
3. Electrocardiogram (ECG): An ECG is a non-invasive test that measures the electrical activity of the heart. It can detect arrhythmias or conduction abnormalities. 4. Echocardiogram: An echocardiogram uses sound waves to create images of the heart’s structure and function. It can identify structural heart abnormalities, such as weakened heart muscle or valve problems.
5. Holter Monitoring: This involves wearing a portable device that records the heart’s electrical activity over a period (usually 24 to 48 hours). It can capture intermittent arrhythmias that may not be detected on a standard ECG.
6. Tilt Table Test: In cases of suspected vasovagal syncope, a tilt table test may be performed to provoke and evaluate syncope under controlled conditions.
Additional tests and evaluations may be recommended based on the individual patient’s presentation and clinical findings.
Management of Syncope in Heart Failure Patients
The management of syncope in patients with heart failure focuses on addressing the underlying cause while also preventing future episodes. Treatment strategies may include:
1. Optimizing Heart Failure Management: This involves ensuring that the patient’s heart failure is adequately controlled with medications, lifestyle modifications, and other therapies to improve cardiac function and reduce symptoms.
2. Medication Adjustment: If syncope is suspected to be related to medication side effects, such as blood pressure-lowering medications, adjustments or changes in medication may be necessary.
3. Implantable Devices: In cases of arrhythmias predisposing to syncope, implantable devices such as pacemakers or defibrillators may be recommended to regulate heart rhythm and prevent sudden cardiac events.
4. Fluid and Electrolyte Balance: Maintaining a proper fluid and electrolyte balance is crucial in heart failure patients to prevent dehydration or electrolyte imbalances that can contribute to syncope.
5. Lifestyle Modifications: Patients may be advised to make lifestyle changes, such as avoiding triggers that can precipitate syncope (e.g., prolonged standing, hot environments) and maintaining regular follow-ups with healthcare providers.
Education and counseling are also essential components of syncope management in heart failure patients. Patients and their caregivers should be educated about recognizing warning signs, adhering to medication regimens, and seeking prompt medical attention if syncope episodes occur.
Conclusion
Syncope can be a complex and multifactorial symptom in patients with heart failure. While it can result from reduced cardiac output, arrhythmias, or medication-related factors, other non-cardiac causes should also be considered during evaluation. A thorough assessment, including medical history, physical examination, and diagnostic tests, is crucial in determining the underlying cause of syncope.